A new Rutgers research study will examine how COVID-19 is affecting people in a number of cognitive-related areas, including memory loss, “brain fog,” and dementia.
” Many individuals who recuperate from mild or moderate COVID-19 notice slowed believing or memory loss, and this inspired us to leverage our experience in studying cognitive problems related to Alzheimers illness, multiple sclerosis, and HIV to analyze this phenomenon,” said Dr. William T. Hu, associate teacher and chief of cognitive neurology at Rutgers Robert Wood Johnson Medical School and the Institute for Health, Healthcare Policy, and Aging Research study.
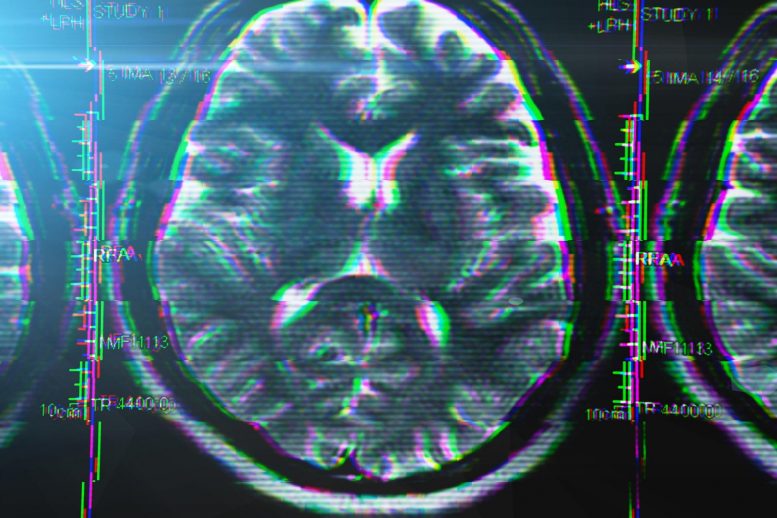
“We developed a roadmap to study the protein and cellular changes included in worsening– as well as minimizing– symptoms of brain fog. Dr. Hus team will evaluate each individuals cognition, mood, and sleep patterns to determine prospective causes of brain fog and compare their brain MRI findings with biochemical signatures of neuroinflammation. They will examine microglial cells– critically essential immune cells in the brain– from individuals who have had COVID-19 to identify whether those cells can be used to predict the determination of post-COVID cognitive impairment (PCCI). We evaluate for all of those things, which helps with total quality of life,” Dr. Hussain described.
A leading cognitive neurologist and neuroscientist, Dr. Hu is leading the characterization of cognitive problems following mild-to-moderate COVID-19 at Rutgers.
” We have discovered neuroinflammation is a typical style throughout numerous brain conditions, however not all neuroinflammation is the very same,” he kept in mind. “We developed a roadmap to study the protein and cellular changes associated with worsening– as well as alleviating– symptoms of brain fog. In addition, we are using the most recent RNA sequencing innovation to understand how inflammatory cells misbehave to trigger memory/thinking dysfunction in long COVID.”
Dr. Hus team will examine each persons cognition, mood, and sleep patterns to identify possible reasons for brain fog and compare their brain MRI findings with biochemical signatures of neuroinflammation. They will evaluate microglial cells– critically crucial immune cells in the brain– from people who have actually had COVID-19 to determine whether those cells can be used to anticipate the determination of post-COVID cognitive disability (PCCI). This will allow researchers to start to produce new hypotheses on why these cells may dysfunction in COVID-19 and PCCI, what the shared inflammatory systems are in between PCCI and Alzheimers illness, and whether FDA-approved drugs can be repurposed to avoid the start of PCCI or enhance its results, Dr. Hu discussed.
Dr. Hu just recently got $100,000 in grant financing from TMCity, a personal foundation based in Irvine, Calif., to assist support the task, which likewise will resolve whether COVID-19 infection accelerates the medical manifestation of Alzheimers disease in people age 50 and above who otherwise would not have demonstrated symptoms up until their 70s and 60s.
“Generous support from TMCity will accelerate this effort in New Brunswick with the capacity of applying the technique more broadly to other organs impacted by long COVID, such as heart and lungs,” Dr. Hu included.
The research study develops on work Dr. Hu and his group have been doing with the growing Post-COVID Recovery Program led by Dr. Sabiha Hussain, associate teacher of medication in the Division of Pulmonary and Critical Care at Rutgers Robert Wood Johnson Medical School. The program, which is a joint effort of the medical school and Robert Wood Johnson University Hospital, typically sees 15-17 people in its weekly Monday centers and supplies a series of services, consisting of behavioral health; cardiology; lung and cardiac rehabilitation; physical, speech and occupational rehabilitation; nutritional services; pulmonary/sleep therapy; and assistance with financial and social barriers connected to recovery, in addition to the cognitive evaluation and treatment that Dr. Hu and his group provide, with additional support in cognitive rehabilitation from the Kessler Institute for Rehabilitation.
Around half of the people who have been seen in the program have problems with brain fog after their bout with COVID. Of those who evaluated positive for neurocognitive concerns, signs include amnesia, brain fog, new confusion, headaches, tingling, and several neurological signs, Dr. Hussain kept in mind.
“Neurocognitive effects of post-COVID syndrome impact the every day life of 62% of our clients,” she stated.
“The vaccine may have assisted somewhat with the brain fog, but what I see from a medical viewpoint is far more persistent short-term amnesia,” included Dr. Hussain, who likewise works as the medical schools director of interventional bronchology, along with its Adult Cystic Fibrosis Program.
She worried that the center is open for anyone who had COVID, no matter whether theyre having active symptoms. “What were finding is that they might not have breathing signs or concerns that would notify them to state, Hey, I require to go see a physician, however they have other underlying signs like a great deal of tiredness, neurocognitive problems, and depression and stress and anxiety that they do not comprehend precisely why it is occurring. We evaluate for all of those things, which helps with overall quality of life,” Dr. Hussain described.
The Post-COVID Recovery Program can be reached at 732-235-7840.