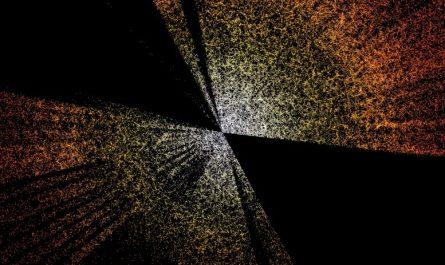
MIT scientists have determined a specialized subset of dendritic cells that help promote T cells to attack growths. In this image, the blue represents a protein discovered on dendritic cell surface areas, and the purple stain reveals tumor proteins that the dendritic cell uses to “disguise” itself as a tumor cell. Cell nuclei are identified in yellow. Credit: Ellen Duong and Tim Fessenden
MIT biologists show that helper immune cells camouflaged as cancer cells can assist rejuvenate T cells that assault growths.
Under the best situations, the bodys T cells can spot and destroy cancer cells. In most cancer patients, T cells become disarmed once they go into the environment surrounding a tumor.
Researchers are now looking for methods to help deal with clients by starting those uninspired T cells. Much of the research study in this field, referred to as cancer immunotherapy, has actually concentrated on discovering ways to stimulate those T cells directly. MIT researchers have actually now discovered a possible brand-new method to indirectly trigger those T cells, by hiring a population of helper immune cells called dendritic cells.
In a new study, the researchers identified a particular subset of dendritic cells that have a special way of triggering T cells. These dendritic cells can mask themselves in tumor proteins, enabling them to impersonate cancer cells and set off a strong T cell response.
” We knew that dendritic cells are extremely important for the antitumor immune action, however we didnt understand what truly makes up the optimal dendritic cell action to a tumor,” states Stefani Spranger, the Howard S. and Linda B. Stern Career Development Professor at MIT and a member of MITs Koch Institute for Integrative Cancer Research.
The results suggest that discovering methods to promote that specific population of dendritic cells could help to boost the efficiency of cancer immunotherapy, she states. In a study of mice, the scientists revealed that stimulating these dendritic cells slowed the growth of melanoma and colon tumors.
Spranger is the senior author of the study, which was published on November 19, 2021, in the journal Immunity. The lead author of the paper is MIT graduate trainee Ellen Duong.
Spontaneous regression
When growths begin to form, they produce malignant proteins that T cells recognize as foreign. This often allows T cells to get rid of tumors before they get very large. In other cases, tumors are able to produce chemical signals that shut down T cells, allowing the growths to continue growing untreated.
Dendritic cells are understood to help trigger tumor-fighting T cells, however there are lots of different subtypes of dendritic cells, and their private roles in T cell activation are not totally identified. In this study, the MIT group wished to investigate which kinds of dendritic cells are included in T cell responses that successfully eliminate growths.
To do that, they discovered a tumor cell line, from a type of muscle growth, that has been revealed to spontaneously fall back in mice. Such cell lines are difficult to discover because researchers usually dont keep them around if they cant form growths, Spranger says.
Studying mice, they compared tumors produced by that regressive cell line with a type of colon carcinoma, which forms tumors that grow bigger after being implanted in the body. The scientists found that in the progressing growths, the T cell reaction quickly became exhausted, while in the falling back tumors, T cells remained functional.
The researchers then evaluated the dendritic cell populations that were present in each of these tumors. One of the primary functions of dendritic cells is to take up debris from dying cells, such as cancer cells or cells contaminated with a pathogen, and after that provide the protein fragments to T cells, alerting them to the infection or growth.
The best-known kind of dendritic cells required for antitumor resistance are DC1 cells, which connect with T cells that have the ability to get rid of cancer cells. The researchers discovered that DC1 cells were not needed for tumor regression. Rather, using single-cell RNA sequencing technology, they identified a formerly unknown activation state of DC2 cells, a different type of dendritic cell, that was driving T cell activation in the regressing growths.
The MIT group found that rather of consuming cellular debris, these dendritic cells swipe proteins called MHC complexes from tumor cells and show them by themselves surfaces. When T cells encounter these dendritic cells masquerading as growth cells, the T cells end up being strongly activated and start eliminating the tumor cells.
This specific population of dendritic cells seems triggered by type one interferon, a signaling molecule that cells typically produce in reaction to viral infection. The scientists found a little population of these dendritic cells in colon and cancer malignancy growths that advance, however they were not properly activated. If they dealt with those growths with interferon, the dendritic cells began stimulating T cells to attack growth cells.
Targeted treatment
Some types of interferon have been used to assist deal with cancer, however it can have widespread side effects when given systemically. The findings from this study suggest that it could be beneficial to provide interferon in an extremely targeted method to tumor cells, or to utilize a drug that would provoke tumor cells to produce type I interferon, Spranger states.
The researchers now plan to examine simply just how much type I interferon is needed to produce a strong T cell response. A lot of growth cells produce a percentage of type I interferon however inadequate to activate the dendritic cell population that stimulates T cells. On the other hand, excessive interferon can be hazardous to cells.
” Our body immune system is hardwired to react to nuanced differences in type I interferon really drastically, and that is something that is appealing from an immunological viewpoint,” Spranger states.
Recommendation: “Type I interferon triggers MHC class I-dressed CD11b+ standard dendritic cells to promote protective anti-tumor CD8+ T cell resistance” by Ellen Duong, Tim B. Fessenden, Emi Lutz, Teresa Dinter, Leon Yim, Sarah Blatt, Arjun Bhutkar, Karl Dane Wittrup and Stefani Spranger, 19 November 2021, Immunity.DOI: 10.1016/ j.immuni.2021.10.020.
The research was funded by the Koch Institute Support (core) Grant from the National Cancer Institute, a National Institutes of Health Pre-Doctoral Training Grant, a David H. Koch Graduate Fellowship, and the Pew-Steward Fellowship.
In this image, the blue represents a protein found on dendritic cell surfaces, and the purple stain reveals growth proteins that the dendritic cell uses to “camouflage” itself as a growth cell. The best-known type of dendritic cells needed for antitumor immunity are DC1 cells, which communicate with T cells that are able to remove cancer cells. Instead, using single-cell RNA sequencing innovation, they determined a formerly unknown activation state of DC2 cells, a different type of dendritic cell, that was driving T cell activation in the regressing tumors.
If they dealt with those tumors with interferon, the dendritic cells started stimulating T cells to assault tumor cells.
Many tumor cells produce a little amount of type I interferon but not adequate to trigger the dendritic cell population that revitalizes T cells.