Jernes hypothesis details a method for the immune system to manage antibodies. It explains a cascade in which the immune system initially launches protective antibody actions to an antigen (like an infection). These secondary antibodies, called anti-idiotype antibodies, can bind to and deplete the preliminary protective antibody reactions.” With the incredible effect of the pandemic and our reliance on vaccines as our main weapon, there is an immense need for more basic science research to comprehend the complex immunological paths at play. This need follows to what it takes to keep the protective actions going, as well as to the possible undesirable side effects of both the infection and the different SARS-CoV-2 vaccine types, specifically as improving is now applied,” Murphy said.
Crucial questions about the infection itself also remain. Approximately one in 4 COVID-19 patients have sticking around symptoms, even after recovering from the virus. These symptoms, referred to as “long COVID,” and the vaccines off-target negative effects are believed to be because of a patients immune action..
In an article published on November 24, 2021, in The New England Journal of Medicine, the UC Davis Vice Chair of Research and Distinguished Professor of Dermatology and Internal Medicine William Murphy and Professor of Medicine at Harvard Medical School Dan Longo present a possible description to the diverse immune actions to the virus and the vaccines..
Antibodies mimicking the virus.
Bring into play classic immunological ideas, Murphy and Longo suggest that the Network Hypothesis by Nobel Laureate Niels Jerne might offer insights..
Jernes hypothesis details a way for the body immune system to regulate antibodies. It explains a cascade in which the body immune system at first releases protective antibody responses to an antigen (like a virus). These exact same protective antibodies later on can set off a brand-new antibody action towards themselves, resulting in their disappearance over time..
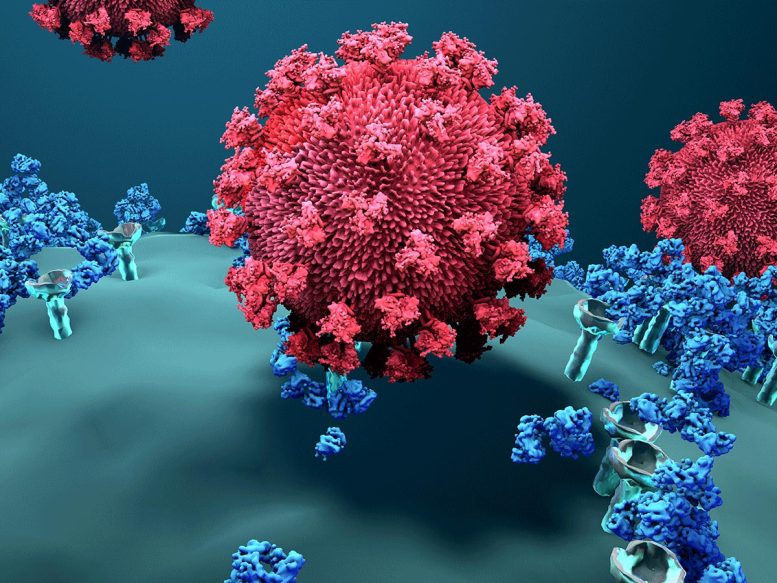
The spike protein mediates the coronavirus entry into host cells.
These secondary antibodies, called anti-idiotype antibodies, can bind to and diminish the initial protective antibody responses. They have the prospective to act or mirror like the original antigen itself. This might lead to negative impacts.
Coronavirus and the body immune system.
When SARS-CoV-2, the infection triggering COVID-19, gets in the body, its spike protein binds with the ACE2 receptor, getting entry to the cell. The body immune system reacts by producing protective antibodies that bind to the getting into infection, blocking or neutralizing its impacts..
As a type of down-regulation, these protective antibodies can likewise cause immune actions with anti-idiotype antibodies. Over time, these anti-idiotype responses can clear the initial protective antibodies and potentially result in limited effectiveness of antibody-based treatments..
” An interesting aspect of the freshly formed anti-idiotype antibodies is that some of their structures can be a mirror image of the original antigen and imitate it in binding to the very same receptors that the viral antigen binds. This binding can possibly lead to undesirable actions and pathology, especially in the long term,” Murphy stated..
The authors recommend that the anti-idiotype antibodies can possibly target the exact same ACE2 receptors. In obstructing or triggering these receptors, they could affect numerous regular ACE2 functions..
” Given the critical functions and large circulation of ACE2 receptors on numerous cell types, it would be essential to identify if these regulatory immune actions might be accountable for some of the long-lasting or off-target effects being reported,” Murphy commented. “These reactions may also discuss why such long-lasting impacts can take place long after the viral infection has passed.”.
As for COVID-19 vaccines, the primary antigen utilized is the SARS-CoV-2 spike protein. According to Murphy and Longo, existing research study studies on antibody actions to these vaccines generally concentrate on the preliminary protective actions and virus-neutralizing efficacy, instead of other long-term elements..
” With the unbelievable impact of the pandemic and our dependence on vaccines as our main weapon, there is an immense need for more standard science research study to comprehend the complex immunological paths at play. This requirement follows to what it takes to keep the protective responses going, in addition to the prospective unwanted side impacts of both the infection and the different SARS-CoV-2 vaccine types, especially as enhancing is now used,” Murphy said. “The great news is that these are testable questions that can be partially addressed in the laboratory, and in truth, have been used with other viral models.”.
Reference: “A Possible Role for Anti-idiotype Antibodies in SARS-CoV-2 Infection and Vaccination” by William J. Murphy, Ph.D. and Dan L. Longo, M.D., 24 November 2021, New England Journal of Medicine.DOI: 10.1056/ NEJMcibr2113694.
With around 256 million cases and more than 5 million deaths worldwide, the COVID-19 pandemic has actually challenged scientists and those in the medical field. Researchers are working to discover efficient vaccines and treatments, in addition to comprehend the long-lasting impacts of the infection..
While the vaccines have been critical in pandemic control, researchers are still learning how and how well they work. This is particularly true with the development of new viral versions and the uncommon vaccine side impacts like allergic reactions, heart inflammation (myocarditis) and blood-clotting (apoplexy)..