Rice University college student Faye Yap, left, and Zhen Liu identify a mask sample. Scientists at Rice and the University of Texas Medical Branch, Galveston, have actually developed a framework for correctly decontaminating non reusable facemasks. They identified that heating a mask in a 160-degrees-Fahrenheit oven for five minutes kills more than 99.9% of the viruses they checked, including SARS-CoV-2. Credit: Jeff Fitlow/Rice University
Heating PPE to the best degree eliminates 99.9% of SARS-CoV-2 virus without breaking down material.
Heres the recipe to decontaminate a disposable facemask: Heat it at 160 degrees Fahrenheit in an oven for five minutes. You can use your own oven.
The science now bears that out, according to engineers at Rice University who, through comprehensive experimentation and modeling, identified that correct heating will get rid of the infection that causes COVID-19 from a standard disposable surgical mask without deteriorating the mask itself.
The work by mechanical engineer Daniel Preston of Rices George R. Brown School of Engineering, Rice college student Faye Yap and partners at the University of Texas Medical Branch (UTMB), Galveston, reveals masks can be decontaminated and reused numerous times before deteriorating.
Most importantly, heating up to 70 degrees Celsius (approximately 160 F) killed more than 99.9% of SARS-CoV-2 and other viruses they evaluated, fulfilling FDA guidelines for decontamination. That shows pledge for adjusting the protocol to manage future break outs where individual protective devices (PPE) is at a premium.
The research study is detailed in the Journal of Hazardous Materials.
Rice University graduate students Faye Yap, left, and Zhen Liu characterize a mask sample. They determined that heating up a mask in a 160-degrees-Fahrenheit oven for 5 minutes kills more than 99.9% of the infections they tested, including SARS-CoV-2.
The paper is the 3rd in a series prompted by the COVID-19 pandemic and supported by a National Science Foundation Rapid Response Research grant. The first paper in August 2020 suggested a thermal method to decontamination would be practical. The 2nd paper, which appeared this May, compared the results of ambient temperature level varies on the virus in numerous U.S. locations.
The current study introduces a modeling structure scientists can utilize to identify just how much heat one needs, and for how long, to kill a particular virus. Preston pointed out the framework applies not just to airborne infections like SARS-CoV-2, however likewise to infections that reside on surfaces and transmit primarily by touch.
In describing their technique, research study authors Yap and Preston detailed decontamination methods that have actually been attempted but just work to a degree: direct exposure to ultraviolet light, since it does not reach into folds or crevices common to masks; steam, due to the fact that it can compromise the structure of a mask; or chemical disinfectants that can leave damaging residues and might also degrade the material.
” In basic, its been shown that ultraviolet light is quite effective, particularly for flat or smooth surface areas,” stated Preston, an assistant professor of mechanical engineering. “Theres a great deal of great out there, however not everybody has access to UV, and heat overcomes the concerns presented by crevices or folds in fabrics.”
When Preston understood little had actually been done to create a modeling framework for decontaminating PPE, he decided his lab was ideal for the task, together with collaborators in Galveston who performed the majority of the heating experiments.
” We actually didnt find anything in the literature that plainly explained the impact of temperature on decontamination of viruses,” he remembered. “At least nothing that could be used to the pandemic. That got us into this even prior to we requested the grant.
Researchers at Rice University and the University of Texas Medical Branch, Galveston, inoculated pieces of basic surgical masks with beads including active viruses to figure out the best approach to decontaminate masks with dry heat. Credit: Jeff Fitlow/Rice University
” Ultimately, what we assumed and have actually now found to be real is that the thermal inactivation of the virus can be quickly described by a mix of two fundamental relationships,” he said. “One of them is the Arrhenius equation, which relates the response parameters to temperature level. And the other is the rate law, which utilizes those reaction specifications to inform you how quick a response takes place. In this case, the response is inactivation of the virus itself.”
Its essential to guarantee the mask warms through, Yap said. Because masks are thin, thats not as much of a concern as decontaminating bigger objects, a topic of future study by the Preston laboratory. Heating to 70 C must work similarly well for fabric masks, as long as all layers reach the required temperature for 5 full minutes.
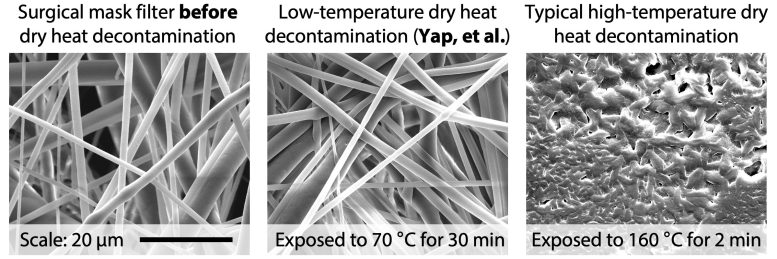
She kept in mind that if the heat is too high, the polymer fibers that make up most masks will melt, as they saw in microscope images of their samples. “At about 125 C, the (middle) filter layer in the mask begins to warp, and at 160 C it melts,” Yap stated. “Theres a great line when you begin to approach the materials melting point.”
But where the decontamination protocol does work, it works extremely well. “If you can get the whole mass to warm up to the correct temperature level, 70 degrees C, then you will still suspend the infections within 5 minutes,” Yap said. Even heating masks to the correct temperature level for approximately 30 minutes did not considerably degrade them, she said.
While COVID-19 is ideally fading in the West, Preston said a scarcity of PPE stays a problem in lots of parts of the world. A simple and reliable approach to decontaminate masks could help numerous. However, the ability to recycle masks is not the be-all and end-all of remaining safe throughout a pandemic.
” I dont desire to claim that thermal inactivation of viruses supported on surface areas is going to be the primary factor to avoiding the spread of COVID-19,” he said. “Viruses are still going to spread through aerosolized beads that transfer from one individual to another. Masks can prevent that, and decontamination represents a secondary safety measure to limit spread.”
Reference: “Efficacy and Self-Similarity of SARS-CoV-2 Thermal Decontamination” by Te Faye Yap, Jason C. Hsu, Zhen Liu, Kempaiah Rayavara, Vivian Tat, Chien-Te, K. Tseng and Daniel J. Preston, 7 November 2021, Journal of Hazardous Materials.DOI: 10.1016/ j.jhazmat.2021.127709.
Jason Hsu of UTMB is co-lead author of the paper. Co-authors are Rice college student Zhen Liu and research scientist Kempaiah Rayavara, college student Vivian Tat and Chien-Te Tseng, a professor of microbiology and immunology, at UTMB.
National Science Foundation grants 2030023 and 2030117 supported the research.
Rice University graduate trainees Faye Yap, left, and Zhen Liu identify a mask sample. They determined that heating a mask in a 160-degrees-Fahrenheit oven for 5 minutes eliminates more than 99.9% of the viruses they tested, including SARS-CoV-2. Rice University graduate students Faye Yap, left, and Zhen Liu define a mask sample. They identified that warming a mask in a 160-degrees-Fahrenheit oven for 5 minutes kills more than 99.9% of the viruses they tested, including SARS-CoV-2. Its essential to make sure the mask warms through, Yap said.