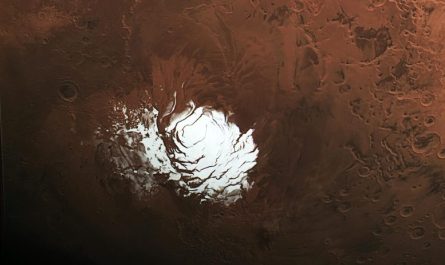
MIT researchers discovered that growth cells from pancreatic cancer clients can exist in 3 states: classical (stained purple and green), basal (stained red), and intermediate (overlapping purple, green and red). Credit: Hannah Williams
Study results likewise show that pancreatic tumor cells can be required into a more prone state by changing their environment.
Over the previous couple of decades, scientists have actually made terrific strides in understanding the hereditary anomalies that can drive cancer. For some types of cancer, these discoveries have led to the advancement of drugs that target specific mutations.
There are still lots of types of cancer for which no such targeted treatments are readily available. A group of scientists from MIT, Dana Farber Cancer Institute, and other organizations is now examining whether another cell characteristic– RNA expression patterns– influences drug actions and can be used to recognize treatments a growth might be prone to.
” What we show in this paper is that cancer cell state is plastic in reaction to the microenvironment and has a significant effect on drug sensitivity. Previous analyses of pancreatic growth cell RNA have actually revealed 2 broad classifications of cell states: basal-like, which is a more aggressive state, and classical. The scientists likewise discovered that the environment in which cancer cells are grown plays a key role in determining their state. The researchers also discovered that they could drive cancer cells, even long-established cell line models, to change in between different states by altering their development conditions. Treating cells with TGF-beta, for example, drives them to a more aggressive, basal-like state, while taking TGF-beta away leads the cells to go back to the classical state in a dish.
In a brand-new study of pancreatic cancer cells, the scientists recognized 3 prototypical RNA-expression states and uncovered differences in their vulnerability to a variety of cancer drugs. They likewise discovered that altering the growth microenvironment can drive tumor cells from one state to another, possibly offering a method to make them more vulnerable to a specific drug.
” What we reveal in this paper is that cancer cell state is plastic in response to the microenvironment and has a remarkable impact on drug level of sensitivity. This opens new frontiers for considering drug development and how to choose drugs for private patients,” states Alex Shalek, a core member of the Institute for Medical Engineering and Science (IMES) at MIT, an associate professor of chemistry, and an extramural member of MITs Koch Institute for Integrative Cancer Research. He is likewise a member of the Ragon Institute of MGH, MIT, and Harvard and an institute member of the Broad Institute.
Shalek and Brian Wolpin, an associate teacher of medicine at Harvard Medical School and Dana-Farber Cancer Institute; William Hahn, a professor of medicine at Harvard Medical School and Dana-Farber; and Andrew Aguirre, an assistant professor of medicine at Harvard Medical School and Dana-Farber; are the senior authors of the research study, which was released on December 9, 2021, in Cell. The papers lead authors are Srivatsan Raghavan, a trainer in medication at Harvard Medical School and Dana-Farber; Peter Winter, an MIT postdoc; Andrew Navia, an MIT college student; and Hannah Williams, a research fellow in medication at Harvard Medical School and Dana-Farber.
Cell states
Sequencing a cells genome can expose cancer-linked mutations, however recognizing these mutations does not always supply information that can be acted on to deal with a particular growth. To generate additional data that might be utilized to assist pick more targeted treatments, Shalek and other scientists have relied on single-cell RNA-sequencing, which reveals the genes that are being expressed by each cell at a minute in time.
” There are a lot of situations where the genes are incredibly crucial, where you can establish these very precise drugs that target translocations or anomalies,” Navia says. “But in lots of instances anomalies alone dont provide you an effective way to target cancer cells relative to healthy ones.”
In this research study, the scientists examined cells from pancreatic ductal adenocarcinoma (PDAC). There are very few targeted drugs readily available to treat pancreatic growths, so most patients get chemotherapy drugs that might be efficient at first but frequently quit working as tumors become resistant. Utilizing single-cell RNA-sequencing, the researchers analyzed about 25 metastatic growth samples from pancreatic cancer patients.
Previous analyses of pancreatic growth cell RNA have actually revealed two broad classifications of cell states: basal-like, which is a more aggressive state, and classical. In the new study, the scientists determined a third state that seems an intermediate between those 2. Cancer cells might travel through this state as they shift from classical to basal-like, the scientists say.
The scientists likewise found that the environment in which cancer cells are grown plays a crucial function in determining their state. In this study, they grew matched “organoids,” or small cancer aggregates from each clients biopsy. Such organoids are typically utilized in accuracy medicine pipelines to model tumors from individual patients, to assist recognize drugs that may be beneficial for those people.
When comparing each in vivo single-cell profile to the matched ex vivo organoid model, the researchers discovered that the organoids often exist in a different RNA state than cancer cells examined straight from the same patient. “We see the same DNA mutations in the original tumor and its model, but when we begin to analyze what they appear like at the RNA level, we discover that theyre very, really various,” Shalek says.
That recommends that the state of a growth can be influenced by the conditions in which its grown rather than its genes alone, he says. The researchers also found that they could drive cancer cells, even long-established cell line models, to change in between different states by changing their development conditions. Dealing with cells with TGF-beta, for instance, drives them to a more aggressive, basal-like state, while taking TGF-beta away leads the cells to go back to the classical state in a meal.
Cells in each of those states depend upon different cell-signaling paths to survive, so knowing the cell state is important to selecting the best kind of drug to deal with a specific growth, the researchers state.
” When we began taking a look at drug level of sensitivity, it became very clear that the same design pushed into a various state would react really in a different way to a drug,” Navia says. “These state-specific sensitivities end up being crucial as we think of preventing and choosing drugs resistance. If you do not understand the ideal state, you could choose the totally wrong compound and try to target the incorrect paths. If you dont think about plasticity, the cancer may only react temporarily until its cells change state.”
Targeted therapy
The findings suggest that more evaluating the interaction of genetics, cell state, and the tumor microenvironment might help researchers to develop new drugs that would efficiently target individual clients tumors.
” Were not removing decades of understanding cancer as a genetic disease, but were definitely stating that we need to much better comprehend the crossway between genes and state,” Winter states. “Cell state absolutely has ties to the underlying level of sensitivity of certain models, and therefore clients and to particular drugs.”
The discovery that cancer cells can be driven from one state to another by customizing the signals in their microenvironment raises the possibility of locking cancer cells into a particular state in a predictable method by therapeutically modifying the growth microenvironment, and after that providing a separate drug to target that locked state and boost treatment effectiveness.
With their coworkers at Dana-Farber, the MIT team is now running much bigger drug screens to determine how each drug impacts pancreatic cancer cells in various states. If those cancer cells are also able to shift between various states in reaction to changes in their microenvironment, they are also studying other types of cancer to identify.
Reference: “Microenvironment drives cell state, plasticity, and drug reaction in pancreatic cancer” by Srivatsan Raghavan, Peter S. Winter, Andrew W. Navia, Hannah L. Williams, Alan DenAdel, Kristen E. Lowder, Jennyfer Galvez-Reyes, Radha L. Kalekar, Nolawit Mulugeta, Kevin S. Kapner, Manisha S. Raghavan, Ashir A. Borah, Nuo Liu, Sara A. Väyrynen, Andressa Dias Costa, Raymond W.S. Ng, Junning Wang, Emma K. Hill, Dorisanne Y. Ragon, Lauren K. Brais, Alex M. Jaeger, Liam F. Spurr, Yvonne Y. Li, Andrew D. Cherniack, Matthew A. Booker, Elizabeth F. Cohen, Michael Y. Tolstorukov, Isaac Wakiro, Asaf Rotem, Bruce E. Johnson, James M. McFarland, Ewa T. Sicinska, Tyler E. Jacks, Ryan J. Sullivan, Geoffrey I. Shapiro, Thomas E. Clancy, Kimberly Perez, Douglas A. Rubinson, Kimmie Ng, James M. Cleary, Lorin Crawford, Scott R. Manalis, Jonathan A. Nowak, Brian M. Wolpin, William C. Hahn, Andrew J. Aguirre and Alex K. Shalek, 9 December 2021, Cell.DOI: 10.1016/ j.cell.2021.11.017.
The research study was funded, in part, by the National Institutes of Health, the Koch Institute and Dana-Farber/Harvard Cancer Center Bridge Project, the Ludwig Center for Molecular Oncology at MIT, the Beckman Young Investigator Program, a Sloan Fellowship in Chemistry, and the Pew-Stewart Scholars Program for Cancer Research.