The Cedars-Sinai private investigators found that individuals with previous infection with SARS-CoV-2, the infection that triggers COVID-19, have a wide range of autoantibodies up to six months after they have completely recovered. To perform their study, the Cedars-Sinai research group hired 177 individuals with validated evidence of a previous infection with SARS-CoV-2. They compared blood samples from these people with samples taken from healthy individuals prior to the pandemic. Some of the autoantibodies also have actually been found in individuals with illness in which the immune system attacks its own healthy cells, such as lupus and rheumatoid arthritis.
Cedars-Sinai Investigators Found Evidence of an Overactive Immune Response.
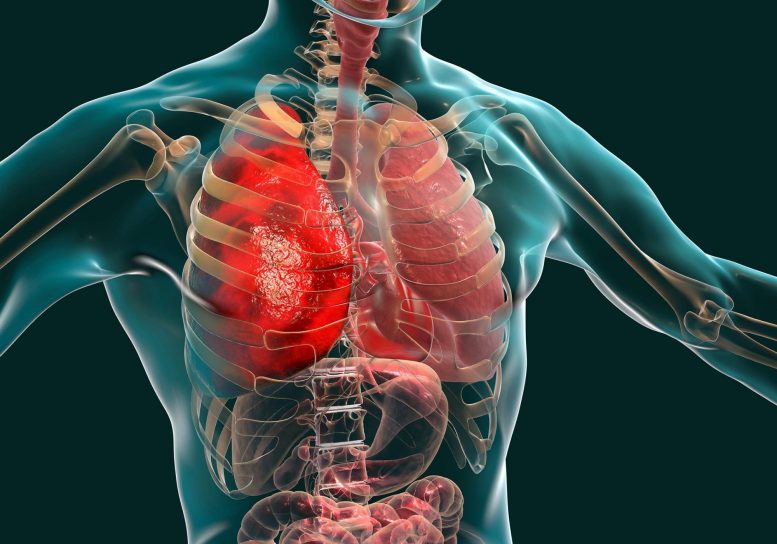
Infection with the virus that triggers COVID-19 can set off an immune response that lasts well beyond the initial infection and recovery– even amongst individuals who had mild signs or no symptoms at all, according to Cedars-Sinai investigators. The findings are published in the Journal of Translational Medicine.
When individuals are contaminated with an infection or other pathogen, their bodies let loose proteins called antibodies that identify foreign compounds and keep them from getting into cells. In many cases, nevertheless, people produce autoantibodies that can attack the bodys own organs and tissues in time.
The Cedars-Sinai detectives discovered that individuals with prior infection with SARS-CoV-2, the infection that causes COVID-19, have a variety of autoantibodies approximately six months after they have completely recuperated. Prior to this study, researchers understood that severe cases of COVID-19 can worry the immune system a lot that autoantibodies are produced. This study is the first to report not just the existence of raised autoantibodies after mild or asymptomatic infection, but their persistence with time.
” These findings help to discuss what makes COVID-19 an especially special disease,” said Justyna Fert-Bober, PhD, research researcher in the Department of Cardiology at the Smidt Heart Institute and co-senior author of the study. “These patterns of immune dysregulation might be underlying the different types of persistent signs we see in individuals who go on to develop the condition now referred to as long COVID-19.”
To conduct their study, the Cedars-Sinai research study group hired 177 people with validated evidence of a previous infection with SARS-CoV-2. Some of the autoantibodies likewise have actually been found in people with diseases in which the immune system assaults its own healthy cells, such as lupus and rheumatoid arthritis.
” We found signals of autoantibody activity that are usually linked to persistent swelling and injury involving specific organ systems and tissues such as the joints, skin and nervous system,” said Susan Cheng, MD, MPH, MMSc, director of the Institute for Research on Healthy Aging in the Department of Cardiology at the Smidt Heart Institute and co-senior author of the study.
Some of the autoantibodies have been linked to autoimmune illness that normally impact ladies regularly than men. In this research study, however, men had a greater variety of elevated autoantibodies than women.
” On the one hand, this finding is paradoxical offered that autoimmune conditions are normally more common in females,” Fert-Bober stated. “On the other hand, it is likewise somewhat expected provided all that we understand about males being more vulnerable to the most serious kinds of COVID-19.”
The research study group is interested in expanding the study to search for the kinds of autoantibodies that may exist and persist in people with long-haul COVID-19 signs. The scientists will likewise examine whether autoantibodies are likewise produced in people with advancement infections since this study was in individuals infected before the arrival of vaccines.
” If we can much better comprehend these autoantibody actions, and how it is that SARS-CoV-2 infection triggers and drives these variable actions, then we can get one step better to identifying methods to treat and even prevent these impacts from developing in people at risk,” Cheng said.
Recommendation: “Paradoxical sex-specific patterns of autoantibody action to SARS-CoV-2 infection” by Yunxian Liu, Joseph E. Ebinger, Rowann Mostafa, Petra Budde, Jana Gajewski, Brian Walker, Sandy Joung, Min Wu, Manuel Bräutigam, Franziska Hesping, Elena Rupieper, Ann-Sophie Schubert, Hans-Dieter Zucht, Jonathan Braun, Gil Y. Melmed, Kimia Sobhani, Moshe Arditi, Jennifer E. Van Eyk, Susan Cheng and Justyna Fert-Bober, 30 December 2021, Journal of Translational Medicine.DOI: 10.1186/ s12967-021-03184-8.