The porcine kidneys are prepared on the backbench for transplant into the brain-dead recipient. Delegated right: Paige Porrett, M.D., Ph.D., Sara Macedon, Natalie Budd, and Jayme Locke M.D. Credit: Photo taken by Jeff Myers, UAB
The surgical team prepares the abdominal area of the brain-dead recipient for xenotransplantation. Left to right: Jayme Locke, M.D., and Natalie Budd, Foreground: Katie Stegner. Credit: Photo taken by Jeff Myers, UAB
Photo shows what the 10-gene modified pig kidney appeared like after reperfusion. The probe is a Doppler that documented excellent signals throughout the kidney. Credit: Photo taken by Jeff Myers, UAB
Genetically customized pig kidneys have actually been thoroughly tested in non-human primates. In addition to testing in non-human primates, evaluating genetically customized pig kidneys in a human preclinical model research study may offer essential information about the potential security and effectiveness of kidneys in human transplant receivers, consisting of in clinical trials.
” This human preclinical model is a method to assess the safety and feasibility of the pig-to-non-human primate design, without risk to a living human,” Locke added. “Our research study demonstrates that major barriers to human xenotransplantation have actually been surmounted, recognizes where brand-new understanding is needed to optimize xenotransplantation outcomes in people, and lays the foundation for the facility of an unique preclinical human model for further study.”
UABs Xenotransplant team. (From left, front row: Jayme Locke, M.D., Katie Stegner, Lindsey Banks, Amy Johnson, M.D., Sara Macedon; Back row: Babak Orandi, M.D., Ph.D., Jordan Lee, M.D., Paige Porrett, M.D., Ph.D., Brett Findley, Natalie Anderson, Drew Shunk, M.D., JennyAnn Eads). Credit: Photo taken by Steve Wood, UAB
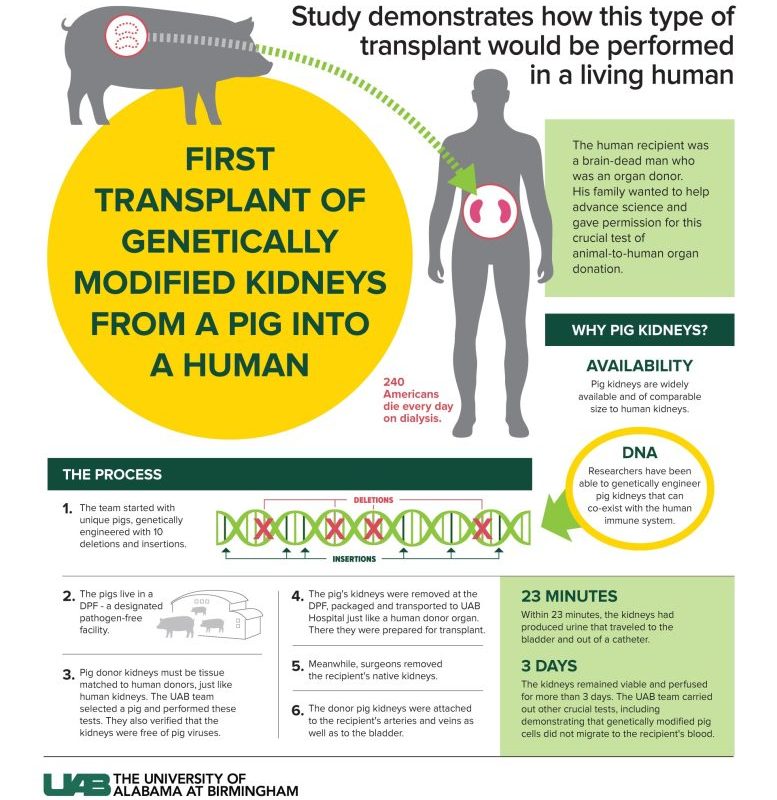
UAB announces very first clinical-grade transplant of gene-edited pig kidneys into brain-dead human.
The study was created and carried out to satisfy requirements directly equivalent to those that would use to a Phase I scientific trial and mirrored– as much as possible– every step of a standard transplant between people.
The University of Alabama at Birmingham Marnix E. Heersink School of Medicine announces today the very first peer-reviewed research study laying out the effective transplant of genetically modified, clinical-grade pig kidneys into a brain-dead human person, replacing the recipients native kidneys. These favorable outcomes demonstrate how xenotransplantation might attend to the around the world organ scarcity crisis.
This effort is supported by biotechnology pioneer United Therapeutics Corporation, which awarded a grant to UAB to launch the ingenious xenotransplantation program. Revivicor, Inc., a subsidiary of United Therapeutics, provided the genetically customized pig that was the source of the investigational xenotransplant kidneys called UKidney ™.
” All of us at Revivicor are in wonder of the historic achievements at UAB with our investigational 10-gene xenokidney, or UKidney,” stated David Ayares, Ph.D., Chief Scientific Officer of Revivicor and a trailblazing genetic engineer since his early work cloning the worlds very first pigs and the very first alpha-Gal knockout pigs. “We feel positive that this UKidney might turn out to be a life-saving option for countless people on dialysis, based on effective conclusion of our clinical trials and achievement of FDA approval in the next a number of years.”
In the research study published in the American Journal of Transplantation, UAB scientists checked the very first human preclinical model for transplanting genetically modified pig kidneys into humans. The study recipient had actually two genetically modified pig kidneys transplanted in his abdominal area after his native kidneys were removed. The organs were obtained from a genetically customized pig at a pathogen-free facility.
” Along with our partners, we have made significant investments in xenotransplantation for almost a years wishing for the kinds of outcomes published today,” said Selwyn Vickers, M.D., dean of the UAB Heersink School of Medicine and CEO of the UAB Health System and UAB/Ascension St. Vincents Alliance. “Todays results are an amazing achievement for humankind and advance xenotransplant into the scientific realm. With this research study, our research study groups have likewise demonstrated that the decedent model has considerable capacity to propel the xenotransplantation field forward.”
This photo reveals what the 10-gene modified pig kidney appeared like prior to reperfusion in the UAB research study. Credit: Photo taken by Jeff Myers, UAB
The surgical team prepares the abdomen of the brain-dead recipient for xenotransplantation. Delegated right: Jayme Locke, M.D., and Natalie Budd Credit: Photo taken by Jeff Myers, UAB
For the very first time, the pig kidneys transplanted were drawn from pigs that had been genetically modified with 10 key gene modifies that may make the kidneys suitable for transplant into human beings. This procedure shows the long-term viability of the treatment and how such a transplant might work in the real life. The transplanted kidneys filtered blood, produced urine and, importantly, were not immediately turned down. The kidneys remained viable up until the research study was ended, 77 hours after transplant.
UABs Xenotransplant team. (From left, front row: Jayme Locke, M.D., Katie Stegner, Lindsey Banks, Amy Johnson, M.D., Sara Macedon; Back row: Babak Orandi, M.D., Ph.D., Jordan Lee, M.D., Paige Porrett, M.D., Ph.D., Brett Findley, Natalie Anderson, Drew Shunk, M.D., JennyAnn Eads). Credit: Photo taken by Steve Wood, UAB
” This game-changing minute in the history of medicine represents a paradigm shift and a major milestone in the field of xenotransplantation, which is perhaps the finest solution to the organ scarcity crisis,” said Jayme Locke, M.D., director of the Comprehensive Transplant Institute in UABs Department of Surgery and lead cosmetic surgeon for the research study. “We have actually bridged important knowledge spaces and acquired the safety and feasibility information necessary to begin a scientific trial in living human beings with end-stage kidney failure disease.”
Gene editing in pigs to minimize immune rejection has actually made organ transplants from pigs to humans possible, which could use assistance to thousands of individuals who face organ disease, injury, or failure. The natural lifespan of a pig is 30 years, they are easily bred and can have organs of similar size to humans.
About the study
The peer-reviewed research is a study of enthusiastic scope and fantastic significance, given that more than 800,000 Americans are dealing with kidney failure. Most never ever make it to the waiting list, and far too few human organs are readily available to put a dent because number. Although dialysis can sustain life for a long time, hair transplant uses a better lifestyle and a longer life for the few people who can get to transplant. Each stage of this decedent xenotransplant study approximated the steps that might be taken in a Phase I xenotransplant medical trial:
Parsons ex-wife, Julie OHara, and their kids, Ally, David, and Cole, made the choice (along with Jims sisters and mom) to participate in the research study after they were approached by Alan Spriggs with Legacy of Hope and Locke.
” Jim was a never-met-a-stranger sort of man who would speak with anybody and had no opponents– none,” OHara said. “Jim would have wanted to save as many people as he might with his death, and if he knew he could potentially conserve thousands and countless people by doing this, he would have had no doubt. Our dream is that no other individual dies awaiting a kidney, and we understand that Jim is extremely happy that his death might potentially bring a lot hope to others.”.
Transplant recipient Jim Parsons assists open doors to the future of organ transplantation
This medical and scientific advancement would not have actually been possible without Jim Parsons, the recipient, or his family.
Parsons, 57, was a signed up organ donor through Legacy of Hope, Alabamas organ procurement organization, and he had actually longed to have his organs help others upon his death; but his organs were not suitable for donation. His family permitted UAB to maintain Parsons on a ventilator to keep his body operating throughout the study. His native kidneys were removed, and two genetically customized pig kidneys were transplanted.
” Mr. Parsons and his household enabled us to replicate specifically how we would perform this transplant in a living human. Their effective contribution will save thousands of lives, which might begin in the really near future,” Locke stated. “Mr. Parsons present honors his tradition and securely establishes the viability, security, and feasibility of this preclinical design. Because of his present, we have actually proposed this to be known as The Parsons Model.”.
The research study was performed to satisfy the standards straight similar to those that would use to a Phase I human clinical trial, matching every action of a basic transplant in between humans. It consisted of Institutional Review Board and Institutional Animal Care and Use Committee approval, a tissue compatibility confirmation prior to starting the operations, utilizing the standard treatments of human-to-human transplants to get rid of, maintain, transportation and transplant the kidneys into a human, and providing the standard immunosuppression treatment to the recipient.
The study recipient had two genetically modified pig kidneys transplanted in his abdomen after his native kidneys were eliminated. For the first time, the pig kidneys transplanted were taken from pigs that had been genetically modified with 10 essential gene modifies that may make the kidneys appropriate for transplant into humans. His native kidneys were removed, and two genetically modified pig kidneys were transplanted.
Kidney illness kills more people each year than breast or prostate cancer, according to the National Institute of Diabetes and Digestive and Kidney Diseases. Hair transplant is the gold standard treatment for end-stage kidney illness, less than 25,000 kidney transplants are performed each year in the United States and 240 Americans on dialysis pass away every day.
The kidneys were gotten rid of from a donor pig housed at a pathogen-free, surgically clean center. The kidneys were then stored, carried, and processed for implantation, just as human kidneys are.
Before surgery, the brain-dead recipient and donor animal underwent a crossmatch compatibility test to determine whether the genetically customized pig kidney and its intended recipient were an excellent tissue match. A crossmatch is provided for every human-to-human kidney transplant; nevertheless, this pig-to-human tissue-match test was established at UAB and marked the first time a potential crossmatch has actually been verified between the two species.
The pig kidneys were positioned in the exact anatomic areas used for human donor kidneys, with the exact same attachments to the renal artery, renal vein and the ureter that brings urine from the kidney to the bladder.
The brain-dead recipient gotten standard immune-suppression therapy utilized in human-to-human kidney allotransplantation.
The crucial requirement for other organ donation alternatives.
Kidney disease kills more people each year than breast or prostate cancer, according to the National Institute of Diabetes and Digestive and Kidney Diseases. Although transplantation is the gold standard treatment for end-stage kidney disease, less than 25,000 kidney transplants are carried out each year in the United States and 240 Americans on dialysis pass away every day. If a limitless supply of kidneys were offered for transplant, many of these deaths could be prevented.
The wait on a departed donor kidney can be as long as 5 years, and in lots of states, it is more detailed to 10 years. Practically 5,000 people per year die waiting on a kidney transplant.
Referral: “First clinical-grade porcine kidney xenotransplant utilizing a human decedent model” 20 January 2022, American Journal of Transplantation.10.1111/ ajt.16930.