” Its essentially an underground kind of transmission,” stated lead author Shan-Lu Liu, a virology teacher in the Department of Veterinary Biosciences at The Ohio State University and a detective in the universitys Center for Retrovirus Research.
” SARS-CoV-2 can spread efficiently from cell to cell since there are basically no blockers from the host resistance. Target cells become donor cells, and it simply becomes a wave of spread, as the infection might not leave the cells.”
Liu and coworkers discovered other revealing details about SARS-CoV-2: The spike protein on its surface area alone makes it possible for cell-to-cell transmission, and yet the infections main receptor on target cells– to which the spike binds– is not a necessary part of the cell-to-cell transmission operation. Furthermore, they discovered that reducing the effects of antibodies are less efficient versus the virus when it spreads through cells.
The research study was released just recently in the journal Proceedings of the National Academy of Sciences.
A significant point of this research study was comparing SARS-CoV-2 to the coronavirus behind the 2003 SARS break out, called SARS-CoV. The findings help discuss why while the very first outbreak led to much greater fatality rates and lasted just 8 months, were about to surpass the two-year mark of the current pandemic, with a bulk of cases being asymptomatic, Liu said.
The comparison revealed that the SARS-CoV that triggered SARS in 2003 is more efficient than SARS-CoV-2 at what is called cell-free transmission, when easily floating viral particles contaminate target cells by binding to a receptor on their surface– however likewise stay susceptible to antibodies produced by previous infection and vaccines. SARS-CoV-2, on the other hand, is more efficient at cell-to-cell transmission– that makes it harder to reduce the effects of with antibodies.
The infections differing efficiencies were first demonstrated in experiments using pseudoviruses– a non-infectious viral core embellished with both kinds of coronavirus spike proteins on the surface area.
” The spike protein is necessary and sufficient for both SARS-CoV-2 and SARS-CoV cell-to-cell transmission because the only difference in these pseudoviruses were the spike proteins,” stated Liu, also a program director of the Viruses and Emerging Pathogens Program in Ohio States Infectious Diseases Institute.
Looking more deeply into those distinctions, the researchers discovered that SARS-CoV-2 is likewise more capable than SARS-CoV at starting fusion with a target cell membrane, another crucial action in the viral entry process. And that more powerful fusion action was associated with the infections enhanced cell-to-cell transmission.
Paradoxically, excessive cell membrane fusion results in cell death and can actually interfere with cell-to-cell transmission, Liu also found.
The team then turned to the role of the ACE2 receptor, a protein on cell surfaces that acts as the entrance for entry of the virus that triggers COVID-19. The scientists discovered, unexpectedly, that cells with no or low levels of ACE2 on their surfaces can be permeated by the virus, allowing robust cell-to-cell transmission.
” There is no ideal connection between SARS-CoV-2 infection and the level of ACE2,” Liu stated. “ACE2 might be required for preliminary infection, once infection is developed, the virus may not need ACE2 anymore since it can spread out from cell to cell.”
Lastly, in experiments evaluating blood samples from human COVID-19 clients against the genuine SARS-CoV-2 infection, scientists determined that the infection could evade an antibody reaction through cell-to-cell transmission, but that antibody neutralization of the virus in the cell-free transmission mode was effective.
” We were able to validate cell-to-cell transmission is not sensitive to inhibition from antibodies from COVID clients or vaccinated individuals,” Liu said. “Cell-to-cell transmissions resistance to antibody neutralization is most likely something we must expect as SARS-CoV-2 versions continue to emerge, including the most current, Omicron. In this sense, establishing reliable antiviral drugs targeting other steps of viral infection is critical.”
There are still lots of unknowns, consisting of the specific mechanism the virus utilizes to spread from cell to cell, how that may influence people reactions to viral infection, and whether or not effective cell-to-cell transmission contributes to the introduction and spread of brand-new versions. Lius laboratory is planning extra research studies utilizing the genuine virus and human lung cells to more check out these questions.
Referral: “SARS-CoV-2 spreads through cell-to-cell transmission” by Cong Zeng, John P. Evans, Tiffany King, Yi-Min Zheng, Eugene M. Oltz, Sean P. J. Whelan, Linda J. Saif, Mark E. Peeples and Shan-Lu Liu, 22 December 2021, Proceedings of the National Academy of Sciences.DOI: 10.1073/ pnas.2111400119.
This work was supported by grants from the National Institutes of Health and funds from an anonymous private donor to Ohio State.
Ohio State co-authors consist of Cong Zeng, Jack Evans, Tiffany King, Yi-Min Zheng, Eugene Oltz, Linda Saif and Mark Peeples, likewise a researcher at Nationwide Childrens Hospital. Sean Whelan of the Washington University School of Medicine likewise contributed.
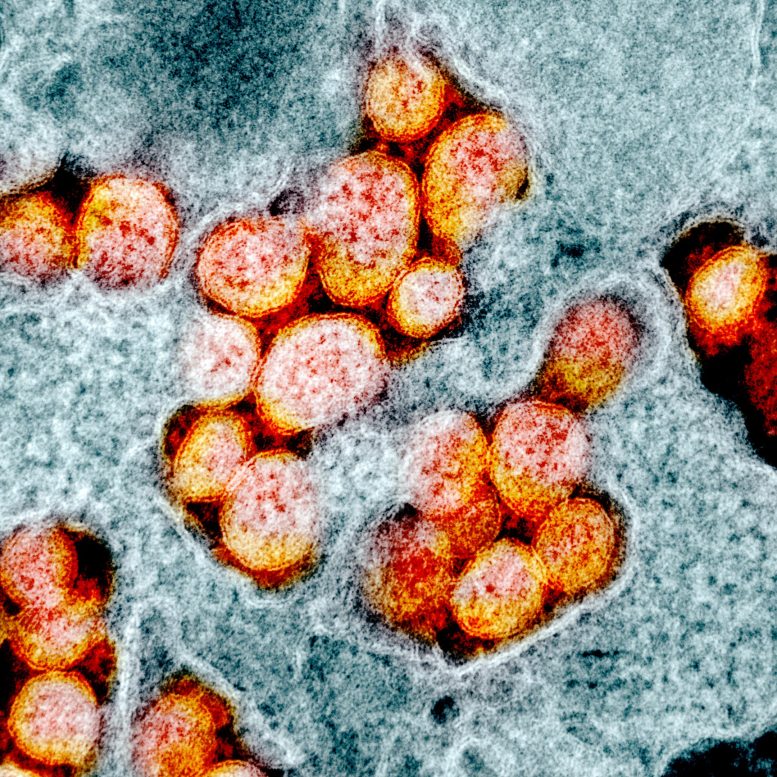
Infections enter cells to make copies of themselves and trigger infection. One trick to SARS-CoV-2s success is concealing from the immune system by spreading out in between cells. This transmission electron micrograph reveals COVID-causing infection particles that were separated from a patient.” We were able to verify cell-to-cell transmission is not sensitive to inhibition from antibodies from COVID patients or immunized people,” Liu said. “Cell-to-cell transmissions resistance to antibody neutralization is probably something we need to view for as SARS-CoV-2 variations continue to emerge, including the most recent, Omicron.
Viruses get in cells to make copies of themselves and trigger infection. One trick to SARS-CoV-2s success is concealing from the immune system by spreading in between cells.
Research study clarifies COVID infection transmissibility, resistance to host immunity.
The infection that triggers COVID-19 has actually embraced some stealth moves to survive and kicking, and one secret to its success is hiding from the body immune system by spreading through cell-to-cell transmission, a new research study has actually found.
Cell culture experiments revealed that SARS-CoV-2, which causes COVID-19, limits the release of viral particles that can be suspended by antibodies, instead remaining tucked within cell walls and spreading out between cells.