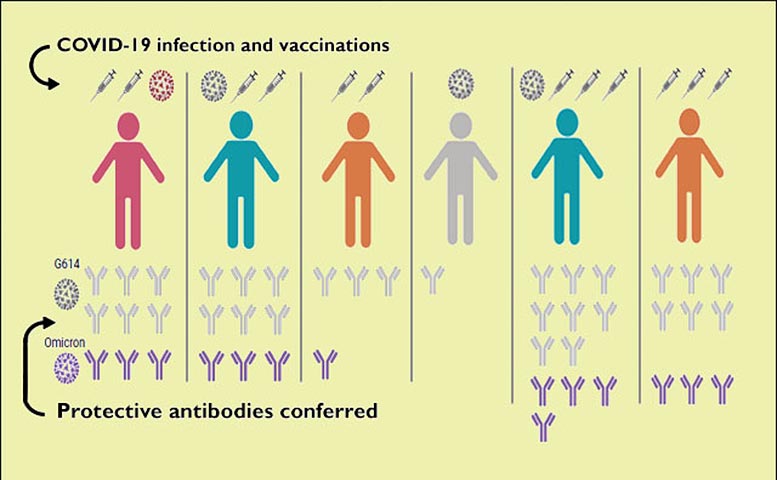
The number of direct exposures to the coronavirus spike protein, through infection or vaccination, affects the degree of antibody action. Credit: Veesler Lab
Individuals vaccinated 3 times or immunized after an earlier COVID-19 infection had equivalent reducing the effects of antibody activity to those with a development case.
A current research study took a look at the strength, toughness, and breadth of neutralizing antibody responses created by breakthrough infections in people immunized against SARS-CoV2.
The findings are published this week in Cell, one of the clinical journals of Cell Press. Alexandra Walls and David Veesler in the Department of Biochemistry at the University of Washington in Seattle led the task.
Characteristics of the Delta and Omicron coronavirus versions of issue include improved transmissibility and immune evasion even in non-immunologically naïve individuals, compared to the ancestral pandemic coronavirus.
These attributes, and the subsiding of resistance from vaccines, have actually resulted in breakthrough infections in vaccinated individuals. For the most part, otherwise healthy people who are immunized versus the SARS-CoV-2 typically do not have serious symptoms if they do wind up contracting the virus.
The researchers wished to comprehend what impact capturing the virus after being immunized has on reducing the effects of antibodies, and to see how long lasting and broad these reactions are. Their hope is that advancing such knowledge will assist vaccination policies and pandemic mitigation strategies.
Through their job the researchers found out that the degree of antibody action depended upon whether an individual has had one, two, 3, or four direct exposures to the spike protein through infection, vaccination, or a mixture of the two. The scientists likewise examined antibody reactions in groups of individuals who had been vaccinated after having COVID-19, those who were previously immunized and experienced a development infection, those who were vaccinated just, and those who were enhanced and therefore immunized 3 times.
Among their research study subjects, those who had actually completed a three-vaccination procedure, and those who had actually been immunized after recovering from COVID-19, and those with a development infection after vaccination launched practically comparable neutralizing antibody responses, in terms of magnitude and breadth. Their serum binding and antibody neutralizing reactions to the spike protein in the existing pandemic coronavirus variants were much more long lasting and powerful than those produced by people who had actually gotten only 2 doses of COVID-19 vaccine or who had a previous infection not followed by vaccination.
This observation recommended that the increased variety of exposures to SARS-CoV-2 antigens, either through infection and vaccination or triple vaccination, enhanced the quality of antibody actions.
The researchers also looked at how broad the elicited antibodies could be. Their findings revealed that increased individuals (or those that have a mixture of infection and double vaccination) have neutralizing antibodies at similar levels to topics immunized twice versus the original ancestral stress.
Looking outside of the SARS-CoV-2 family reveals a comparable pattern, where repeated and several exposures enhances the otherwise weak neutralizing antibody reaction to SARS-CoV. The authors did not recognize improvements in antibody binding to common cold triggering coronavirus spike proteins like OC43 or HKU1. This recommends that duplicated SARS-CoV-2 direct exposure does not enhance spike reactivity to more divergent coronaviruses. These findings support the advancement of more comprehensive sarbecovirus or coronavirus vaccines to be prepared in the occasion of a future spillover event.
The research study groups consisted of about 15 people, from the Hospitalized or Ambulatory Adults with Respiratory Viral Infections, or HAARVI, job at the UW in Seattle. HAARVI, led by UW Medicine infectious disease doctor Helen Chu, takes a look at recuperated COVID-19 clients to study immune actions over time, to understand the long-term repercussions of the infection, and to compare immune reactions from vaccines and natural infections.
Reference: “SARS-CoV-2 breakthrough infections generate potent, broad and durable neutralizing antibody reactions” by Alexandra C. Walls, Kaitlin R. Sprouse, John E. Bowen, Anshu Joshi, Nicholas Franko, Mary Jane Navarro, Cameron Stewart, Elisabetta Cameroni, Matthew McCallum, Erin A. Goecker, Emily J. Degli-Angeli, Jenni Logue, Alex Greninger, Davide Corti, Helen Chu and David Veesler, 19 January 2022, Cell.DOI: 10.1016/ j.cell.2022.01.011.
Researchers from the Department of Medicine and the Department of Laboratory Medicine and Pathology at the UW School of Medicine, and from Humabs Biomed SA, a subsidiary of Vir Biotechnology, likewise helped conduct the research study.
The researchers also looked at how broad the elicited antibodies could be. Their findings showed that enhanced individuals (or those that have a mixture of infection and double vaccination) have reducing the effects of antibodies at comparable levels to topics vaccinated two times versus the original ancestral pressure. This recommends a large quantity of immune evasion, however that vaccine boosters can assist close the neutralizing antibody gap caused by Omicron.
Looking outside of the SARS-CoV-2 household shows a comparable pattern, where duplicated and several exposures improves the otherwise weak reducing the effects of antibody action to SARS-CoV. The authors did not recognize enhancements in antibody binding to typical cold triggering coronavirus spike proteins like OC43 or HKU1.