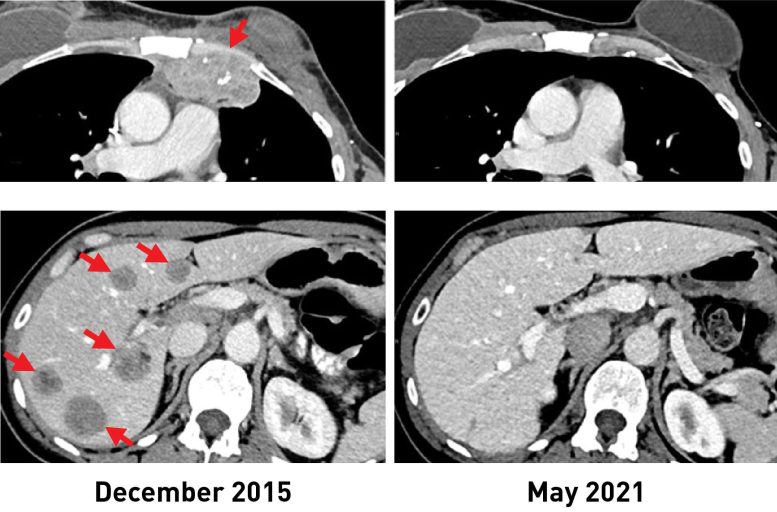
Woman with breast cancer had metastatic lesions in chest wall (top, left) and liver (bottom, left). After receiving the immunotherapy, tumors shrank entirely. Current scans (R) reveal she is cancer totally free more than 5 years later on. Credit: The National Cancer Institute (NCI).
A speculative type of immunotherapy that uses an individuals own tumor-fighting immune cells could potentially be used to treat people with metastatic breast cancer, according to results from a continuous scientific trial led by researchers at the National Cancer Institutes (NCI) Center for Cancer Research, part of the National Institutes of Health. Many individuals with metastatic breast cancer can mount an immune response against their growths, the research study found, a prerequisite for this type of immunotherapy, which relies on what are called tumor-infiltrating lymphocytes (TILs).
In a scientific trial of 42 ladies with metastatic breast cancer, 28 (or 67%) produced an immune reaction versus their cancer. The method was utilized to treat six females, half of whom experienced quantifiable growth shrinkage. Arise from the trial appeared Feb. 1, 2022, in the Journal of Clinical Oncology.
” Its popular dogma that hormonal agent receptor– favorable breast cancers are not efficient in provoking an immune action and are not prone to immunotherapy,” stated study leader Steven A. Rosenberg, M.D., Ph.D., chief of the Surgery Branch in NCIs Center for Cancer Research. “The findings suggest that this form of immunotherapy can be utilized to treat some people with metastatic breast cancer who have actually exhausted all other treatment options.”.
Female with breast cancer had metastatic lesions in chest wall (top, left) and liver (bottom, left). In a clinical trial of 42 females with metastatic breast cancer, 28 (or 67%) created an immune reaction against their cancer. Other forms of immunotherapy have actually been discovered to be efficient in treating cancers, such as cancer malignancy, that have lots of anomalies, and therefore many neoantigens. This trial was developed to see if the immunotherapy technique might lead to growth regressions in individuals with metastatic epithelial cancers, consisting of breast cancer. Those women now have no proof of cancer approximately 5 years and 3.5 years, respectively, after their TIL treatment.
Immunotherapy is a treatment that helps a persons own immune system battle cancer. Nevertheless, most readily available immunotherapies, such as immune checkpoint inhibitors, have revealed limited effectiveness versus hormonal agent receptor– positive breast cancers, which are the majority of breast cancers.
The immunotherapy technique utilized in the trial was originated in the late 1980s by Dr. Rosenberg and his colleagues at NCI. It counts on TILs, T cells that are discovered around the tumor.
TILs can target growth cells that have particular proteins on their surface area, called neoantigens, that the immune cells acknowledge. When anomalies occur in growth DNA, neoantigens are produced. Other types of immunotherapy have actually been found to be effective in treating cancers, such as melanoma, that have numerous anomalies, and for that reason numerous neoantigens. Its effectiveness in cancers that have less neoantigens, such as breast cancer, nevertheless, has been less clear..
The outcomes of the new study originated from a continuous stage 2 scientific trial being carried out by Dr. Rosenberg and his coworkers. This trial was developed to see if the immunotherapy approach could cause growth regressions in people with metastatic epithelial cancers, consisting of breast cancer. In 2018, the researchers showed that a person female with metastatic breast cancer who was dealt with in this trial had complete tumor shrinkage, referred to as a total action.
In the trial, the researchers utilized whole-genome sequencing to determine anomalies in growth samples from 42 females with metastatic breast cancer whose cancers had actually progressed despite all other treatments. The scientists then separated TILs from the tumor samples and, in lab tests, checked their reactivity against neoantigens produced by the different anomalies in the tumor.
Twenty-eight ladies had TILs that recognized at least one neoantigen. Nearly all the neoantigens identified were unique to each patient.
” Its fascinating that the Achilles heel of these cancers can possibly be the very gene mutations that triggered the cancer,” said Dr. Rosenberg. “Since that 2018 study, we now know on 42 patients, revealing that the bulk trigger immune reactions.”.
For the 6 females dealt with, the scientists took the reactive TILs and grew them to great deals in the laboratory. They then returned the immune cells to each patient by means of intravenous infusion. All the patients were likewise provided four dosages of the immune checkpoint inhibitor pembrolizumab (Keytruda) prior to the infusion to avoid the newly introduced T cells from ending up being inactivated.
After the treatment, growths shrank in 3 of the six females. One is the initial female reported in the 2018 research study, who stays cancer free to this day. The other two females had growth shrinkage of 52% and 69% after 6 months and 10 months, respectively. However, some disease returned and was surgically removed. Those women now have no proof of cancer around 5 years and 3.5 years, respectively, after their TIL treatment.
The researchers acknowledged that making use of pembrolizumab, which has been approved for some early-stage breast cancers, may raise uncertainties about its influence on the outcome of TIL therapy. They said, treatment with such checkpoint inhibitors alone has not led to sustained tumor shrinking in people with hormonal agent receptor– favorable metastatic breast cancer.
Dr. Rosenberg said that with the anticipated opening early this year of NCIs brand-new structure devoted to cell-based therapies, he and his coworkers can begin dealing with more people with metastatic breast cancer as part of the ongoing scientific trial. He noted that this brand-new immunotherapy method might possibly be used for people with other types of cancer.
” Were using a patients own lymphocytes as a drug to deal with the cancer by targeting the distinct anomalies in that cancer,” he stated. “This is an extremely individualized treatment.”.
Reference: “Breast Cancers are immunogenic: Immunologic analyses and a phase II pilot medical trial utilizing mutation-reactive lymphocytes” 1 February 2022, Journal of Clinical Oncology.