” We understand that for the majority of kids with PBB, their cough will get better after they have had a two-week course of prescription antibiotics, but we also know that some kids will have duplicated episodes of bronchitis that never ever appear to get much better,” Dr. Marsh stated.
” This puts them at danger of establishing an extreme lung illness called bronchiectasis. We know that chest infections can cause PBB and bronchiectasis, but the reasons just some kids react to prescription antibiotics isnt constantly clear.”.
The research study group used a procedure called bronchoalveolar lavage (BAL) to collect a sample from the lungs for testing. During the treatment, a sterile service is utilized to flush the childs respiratory tracts and catch a fluid sample consisting of the bacteria that cause the kids chest infection. This is the very first known study to demonstrate a prevalence of biofilm in affected children.
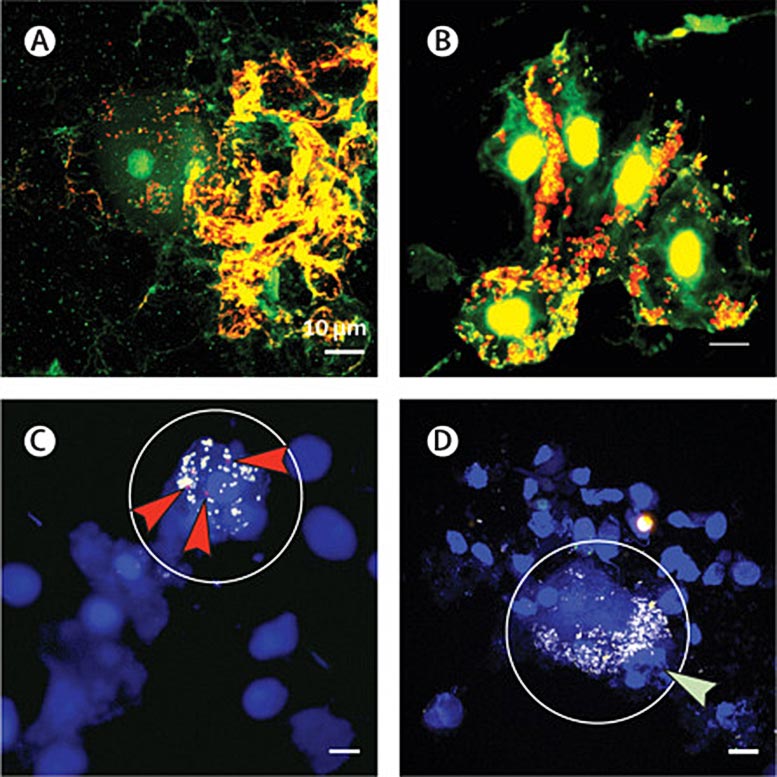
Research study co-author Dr. Ruth Thornton a Research Fellow, UWA Centre for Child Health Research (associated with the Telethon Kids Institute) states utilizing the effective microscope with contrasting colors helped in locating and identifying the bacterial slime which exists in the affected lungs.
” This is an important discovery as we understand that when germs live in these slimes they can be more than a thousand times more resistant to antibiotics than the bacteria that trigger the intense infections that you take your kid to the doctor for. This means that when you stop antibiotics your child is most likely to get yet another infection,” Dr. Thornton said.
Professor Anne Chang AM, Menzies Head of Child Health explained the study results as an amazing way forward to assist treat the children who have actually been suffering.
” This is truly interesting. Weve believed these kids have biofilm-associated infections for a while however up until now, no one has actually proven it. Now that weve seen it, we can begin investigating new methods to deal with these kids so that fewer of them will advance to having serious lung illness,” Prof Chang stated.
Referral: “Prevalence and subtyping of biofilms present in bronchoalveolar lavage from kids with lengthy bacterial bronchitis or non-cystic fibrosis bronchiectasis: a cross-sectional research study” by Robyn L Marsh, PhD; Michael J Binks, PhD; Heidi C Smith-Vaughan, PhD; Maxine Janka, BSc; Sharon Clark, BBioMedSc; Prof Peter Richmond, MD; Prof Anne B Chang, PhD and Ruth B Thornton, PhD, 1 February 2022, The Lancet Microbe.DOI: 10.1016/ S2666-5247( 21 )00300-1.
Menzies School of Health Research.
Menzies is one of Australias leading medical research study institutes dedicated to improving the health and wellbeing of Aboriginal and Torres Strait Islanders, and a leader in tropical and global research into lethal health problems, Menzies continues to equate research into reliable partnerships and programs in neighborhoods throughout Australia and the Asia-Pacific area.
(A) BacLight-stained bronchoalveolar lavage from a kid with lengthy bacterial bronchitis (PBB) showing big biofilms containing dead and live germs connected to squamous epithelial cells. (B) BacLight-stained bronchoalveolar lavage from a kid with bronchiectasis revealing dead and live bacteria in biofilms attached to squamous epithelial cells. (C) FISH-stained bronchoalveolar lavage from a kid with PBB showing a squamous epithelial cell (SEC) biofilm containing little clusters of Moraxella catarrhalis (red arrows) and other unidentified bacteria (eubacterial probe in yellow) associated with host DNA (blue). (D) FISH-stained bronchoalveolar lavage from a child with bronchiectasis revealing a SEC biofilm that is favorable for Streptococcus pneumoniae (green arrow) and other unknown germs (eubacterial probe in yellow) associated with host DNA (blue). During the procedure, a sterilized option is used to flush the childs airways and record a fluid sample including the bacteria that trigger the kids chest infection.
Squamous epithelial cell biofilms observed in bronchoalveolar lavage from children with drawn-out bacterial bronchitis or bronchiectasis. Agent maximum intensity projections of bronchoalveolar lavage stained with BacLight (A– B), fluorescent in situ hybridization (FISH) probes (C– D), or hematoxylin and eosin (E– F). In BacLight images, DNA within undamaged (live) bacteria is stained green whereas extracellular DNA and permeable (dead) bacteria are stained red. (A) BacLight-stained bronchoalveolar lavage from a kid with lengthy bacterial bronchitis (PBB) showing large biofilms containing dead and live bacteria connected to squamous epithelial cells. (B) BacLight-stained bronchoalveolar lavage from a kid with bronchiectasis revealing dead and live bacteria in biofilms connected to squamous epithelial cells. (C) FISH-stained bronchoalveolar lavage from a kid with PBB showing a squamous epithelial cell (SEC) biofilm including little clusters of Moraxella catarrhalis (red arrows) and other unidentified bacteria (eubacterial probe in yellow) connected with host DNA (blue). The circle suggests the associated squamous epithelial cell. No non-specific hybridization (NONEUB probe in green) was observed. (D) FISH-stained bronchoalveolar lavage from a child with bronchiectasis showing a SEC biofilm that is favorable for Streptococcus pneumoniae (green arrow) and other unidentified germs (eubacterial probe in yellow) associated with host DNA (blue). The circle indicates the associated squamous epithelial cell. Credit: The Lancet Microbe, DOI: 10.1016/ S2666-5247( 21 )00300-1.
New research study has led to a development in comprehending an essential motorist of frequent chest infections in children.
Lots of children experience an extended damp cough after having a severe cough and can establish a condition called protracted bacterial bronchitis or PBB. In a collaborative study published in the prestigious The Lancet Microbe journal, scientists from Menzies School of Health Research (Menzies), The Telethon Kids Institute and the University of Western Australia (UWA) used a powerful microscopic lense to discover that some of the kids with consistent wet coughs had a bacterial slime– called a biofilm– in their lungs.
Lead author, Menzies Senior Research Fellow, Dr. Robyn Marsh states kids with persistent PBB are at increased danger of progressing to a severe lung illness called bronchiectasis.