” When it concerns drug delivery, the issue, as molecular biologist Inder Verma put it, is delivery, shipment, and shipment,” explained Yamuna Krishnan, a professor in the Department of Chemistry and an author of the study. “These DNA nanodevices now make drug shipment hyperspecific, enabling us to think about methods to treat cancer without eliminating the cell that the restorative is delivered to.”
The focus of these nanodevices is a particular type of cell referred to as tumor-associated macrophages, or TAMs. Macrophages are a kind of immune cell that generally is supposed to acknowledge and eliminate microbes, cellular particles, and other foreign compounds from cells; however if something fails with them, they can become a crucial part of cancerous growths. TAMs can comprise approximately 50% of growth mass in triple-negative breast cancer.
“despite the high abundance of TAMs in strong tumors, mechanisms underlying their effect on tumor development and healing strategies to target them are incompletely comprehended,” said research study co-author Lev Becker, associate professor in the Ben May Department for Cancer Research.
The importance of these TAMs returns to how the immune system acknowledges cancerous cells. There is a subpopulation of immune cells called CD8+ T cells that are critical in acknowledging and eliminating malignant cells. These CD8+ T cells can be triggered against dangers by binding to molecular structures called “antigens” on the surface of malignant macrophages. This technique goes awry, however, when TAMs do not present antigens, so there is nothing for the T-cells to acknowledge.
Beckers group discovered that TAMs harbored a high level of a kind of enzyme called cysteine proteases. They knew these particular enzymes live in lysosomes, which work as the “stomach” of the cell, so Beckers insight was that they might be “over-digesting” tumor antigens– therefore hiding cancerous cells from patrolling CD8+ T cells.
They found that undoubtedly, the lysosomes in the TAMs of these mice werent ruining antigens as much. This ultimately enabled CD8+ T cells to “see” and assault the growth.
Next, they needed to find out a way to target this process therapeutically.
” Our intent was not to kill the target cells, however rather reprogram them and alter their character.”
— Prof. Yamuna Krishnan
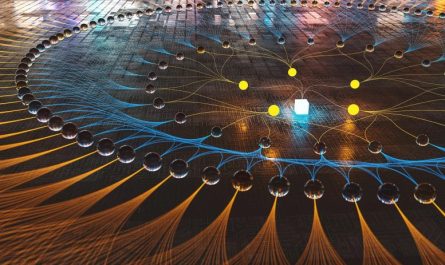
Krishnan, a specialist in DNA nanotechnology, had actually recently developed the expertise to send out tiny nanodevices made out of DNA directly to the lysosomes of specific immune cells in design organisms such as worms and zebrafish. The 2 labs collaborated to conquer this obstacle.
Kasturi Chakraborty, a previous college student of the Krishnan lab and now a postdoctoral scholar in Beckers lab, established a tiny DNA nanodevice that provided a cysteine protease inhibitor. When Chang Cui, a graduate trainee in the Becker lab, injected it into a mouse with a tumor, this nanodevice preferentially targeted lysosomes inside TAMs, where it stopped the enzymes from damaging antigens– rendering them when again “visible” to patrolling immune cells.
Combining this DNA nanodevice with frontline chemotherapy resulted in sustained tumor regression in a triple-negative-breast-cancer design in tests with mice. Due to the fact that this type of cancer is especially tough to treat, this outcome was amazing.
Its also a fundamentally different approach from the standard manner in which researchers think of dealing with cancer: “When we target a drug, success normally implies you have actually eliminated the cell you wished to target,” stated Krishnan. “However, in our technique, our intent was not to kill the target cells, however rather reprogram them and alter their character. As soon as the nanodevice flips the switch in a TAM, natural immunity looks after the rest.”
The scientists hope that this new organelle-specific delivery using DNA nanodevices is the next generation of drug targeting.
It might even exceed cancer, because specific delivery to macrophages could affect a broad series of diseases where immunity has gone awry, the researchers said.
” You wouldnt see this operate in just a chemistry laboratory or just an immunology lab,” stated Chakraborty. “At UChicago, biologists and chemists are in the exact same building, so there is a simple circulation of interactions and the environment actually motivates interdisciplinary science.”
Referral: “A lysosome-targeted DNA nanodevice selectively targets macrophages to attenuate tumours” by Chang Cui, Kasturi Chakraborty, Xu Anna Tang, Kelly Q. Schoenfelt, Alexandria Hoffman, Ariane Blank, Blake McBeth, Natalie Pulliam, Catherine A. Reardon, Swati A. Kulkarni, Tomas Vaisar, Andrea Ballabio, Yamuna Krishnan and Lev Becker, 11 November 2021, Nature Nanotechnology.DOI: 10.1038/ s41565-021-00988-z.
Financing: Womens Board Faculty Research Startup Funds, Ben May Department Startup Funds (L.B.), the University of Chicago Womens Board (Y.K.).
A team of University of Chicago chemists and biologists established a tiny gadget that can find tumor cells and require them to expose themselves to patrolling immune cells. The focus of these nanodevices is a particular type of cell understood as tumor-associated macrophages, or TAMs. Macrophages are a type of immune cell that generally is supposed to recognize and remove microorganisms, cellular particles, and other foreign compounds from cells; however if something goes incorrect with them, they can become a crucial part of malignant growths. There is a subpopulation of immune cells called CD8+ T cells that are crucial in acknowledging and eliminating cancerous cells. Its likewise a fundamentally various approach from the basic way that scientists think about treating cancer: “When we target a drug, success normally suggests you have actually killed the cell you desired to target,” said Krishnan.
Early tests at UChicago show promise for dealing with resistant tumors with special technique.
Among the most appealing opportunities in dealing with cancer is to restore our body immune systems capability to recognize and assault cancerous cells. A group of University of Chicago chemists and biologists established a tiny device that can find tumor cells and force them to reveal themselves to patrolling immune cells. In tests with mice, this led to tumor regression.