SALL4 is a recognized oncogene, and the expression of SALL4 has actually been found to contribute to the advancement of MDS and leukemia. A research study performed by another research group in 2016 showed that SALL4 activation in a liver cancer cell line was associated with hypomethylation, and Professor Daniel Tenen from CSI Singapore and his team showed in 2021 that hepatitis B virus induced SALL4 demethylation in liver cancer through an RNA mediated system. To analyze possible upregulation of oncogenes in patients being treated with hypomethylating representatives, Professor Tenens group collaborated with the other groups to study the association between HMA made use of and SALL4 activation, as well as the implications on survival outcomes.
While upregulation of SALL4 might likely influence the illness progression and be associated with a poorer medical diagnosis, it may also supply an opportunity to identify patients for early intervention with a drug targeting SALL4 pathways, therefore enhancing treatment and patient outcomes,” said Professor Tenen.
Switching on the gene that triggers cancer
SALL4 is a known oncogene, and the expression of SALL4 has actually been found to contribute to the advancement of MDS and leukemia. A study performed by another research group in 2016 showed that SALL4 activation in a liver cancer cell line was associated with hypomethylation, and Professor Daniel Tenen from CSI Singapore and his team showed in 2021 that hepatitis B virus caused SALL4 demethylation in liver cancer through an RNA mediated system. To examine possible upregulation of oncogenes in clients being treated with hypomethylating agents, Professor Tenens team collaborated with the other groups to study the association in between HMA used and SALL4 activation, in addition to the implications on survival results.
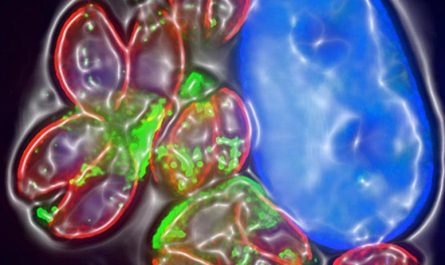
The research group analyzed the bone marrow samples of 68 clients with MDS, taken before and after their HMA treatment. The scientists discovered that HMA therapy could result in the activation of the SALL4 oncogene, causing poor survival results for clients, even those in total disease remission.
” Our findings from this pioneering research study reveal that treatment utilizing hypomethylating agents can activate and upregulate oncogenes, such as SALL4. This recommends the significance of keeping an eye on SALL4 expression levels in clients getting HMA therapy. While upregulation of SALL4 may likely affect the disease progression and be associated with a poorer medical diagnosis, it may also provide an opportunity to determine patients for early intervention with a drug targeting SALL4 paths, therefore improving treatment and client results,” stated Professor Tenen.
Early intervention for better results
Interestingly, these findings by Professor Tenens group, dealing with the BWH and HMS groups, more support another research study of theirs in 2021, in which they demonstrated that cancer cells with reactivated SALL4 by hypomethylation were efficiently treated with a drug created to prevent a SALL4 downstream path. These newly established concepts might help modify the treatment paradigm for other cancers and diseases where HMAs are being utilized.
Moving on, the group means to perform bigger prospective studies to verify these findings and develop precise however low-cost biomarkers kits to monitor SALL4 expression. Through collaborative research study throughout laboratories, the group aims to develop more reliable and specific drugs that target SALL4 directly.
Referral: “Demethylation and Up-Regulation of an Oncogene after Hypomethylating Therapy” by Yao-Chung Liu, M.D., Junsu Kwon, Ph.D., Emiliano Fabiani, Ph.D., Zhijian Xiao, M.D., Yanjing V. Liu, Ph.D., Matilde Y. Follo, Ph.D., Jinqin Liu, M.D., Huijun Huang, M.D., Chong Gao, M.D., Jun Liu, M.D., Giulia Falconi, Ph.D., Lia Valentini, M.S., Carmelo Gurnari, M.D., Carlo Finelli, M.D., Lucio Cocco, M.D., Jin-Hwang Liu, Ph.D., Adrianna I. Jones, B.S., Junyu Yang, Ph.D., Henry Yang, Ph.D., Julie A.I. Thoms, Ph.D., Ashwin Unnikrishnan, Ph.D., John E. Pimanda, M.D., Rongqing Pan, Ph.D., Mahmoud A. Bassal, Ph.D., Maria T. Voso, M.D., Daniel G. Tenen, M.D. and Li Chai, M.D., 26 May 2022, New England Journal of Medicine.DOI: 10.1056/ NEJMoa2119771.
Scientists found that hypomethylating agents, a medication typically used to deal with myelodysplastic syndrome, might “turn on” the gene that causes cancer.
Scientists propose a method for early intervention to enhance treatment outcomes
Hypomethylating representatives (HMA) are presently used as a first-line treatment for people with myelodysplastic syndrome (MDS), a group of conditions where there is an insufficient generation of healthy mature blood cells in the bone marrow. However, the precise system through which HMAs work is still unidentified. This has actually not yet been totally shown, one possible concern is that they might trigger a sleeping oncogene.
In a recent study, scientists from the National University of Singapores (NUS) Cancer Science Institute of Singapore (CSI Singapore) in close cooperation with Bostons Brigham and Womens Hospital (BWH) and Harvard Medical School (HMS) have revealed that HMAs can and do trigger the oncofetal protein SALL4.
The research study was published in the academic journal New England Journal of Medicine and was also performed in collaboration with the University of Tor Vergata in Rome, Italy, and the Institute of Hematology and Blood Diseases Hospital in Tianjin, China.