” The outcomes of our examination aid describe why the hereditary links to Crohns illness are much more comprehensive than the real variety of individuals who have the disease.”– Shohei Koide, PhD
” The outcomes of our examination aid describe why the genetic links to Crohns illness are much wider than the real variety of people who have the illness,” says Shohei Koide, PhD, the studys co-senior author and a biochemist. Dr. Koide is a professor in the Department of Biochemistry and Molecular Pharmacology and a member of Perlmutter Cancer Center at NYU Langone.
” Our study suggests that when norovirus contaminates those with a weakened ability to produce apoptosis inhibitor 5, it ideas the balance towards a full-blown autoimmune disease,” includes study co-senior author and microbiologist Ken H. Cadwell, PhD, the Recanati Family Professor of Microbiology at NYU Langone.
Dr. Cadwell warns that while the study authors obtained API5 protein from human tissue rather than rodents, it stays uncertain whether the injection treatment can be safely administered in people.
Next, the research study group prepares to check out the long-lasting impacts of API5 injections to better understand whether the prospective treatment can efficiently manage Crohns illness, which can flare consistently over an extended period.
Recommendation: “The γδ IEL effector API5 masks hereditary susceptibility to Paneth cell death” by Yu Matsuzawa-Ishimoto, Xiaomin Yao, Akiko Koide, Beatrix M. Ueberheide, Jordan E. Axelrad, Bernardo S. Reis, Roham Parsa, Jessica A. Neil, Joseph C. Devlin, Eugene Rudensky, M. Zahidunnabi Dewan, Michael Cammer, Richard S. Blumberg, Yi Ding, Kelly V. Ruggles, Daniel Mucida, Shohei Koide and Ken Cadwell, 5 October 2022, Nature.DOI: 10.1038/ s41586-022-05259-y.
In addition to Dr. Matsuzawa-Ishimoto, Dr. Koide, and Dr. Cadwell, other NYU Langone private investigators included in the study were Xiaomin Yao, PhD; Akiko Koide, PhD; Beatrix M. Ueberheide, PhD; Jordan E. Axelrad, MD, MPH; Jessica Neil, PhD; Joseph Devlin, PhD; Eugene Rudensky, PhD; M. Zahidunnabi Dewan, PhD; Michael Cammer, PhD; Kelly V. Ruggles, PhD; and Daniel Mucida, PhD. Other study investigators were Bernardo Reis, PhD, and Roham Parsa, PhD, at The Rockefeller University in New York City; Richard Blumberg, PhD, at Harvard Medical School in Boston; and Yi Ding, PhD, at Geisinger Health in Danville, Pennsylvania.
Funding for the study was supplied by National Institutes of Health grants R0IL123340, R0IDK093668, R0IAI140754, R0IAI121244, R0IAI130945, R0IDK124336, and R0IDK088199. Further funding was provided by the Howard Hughes Medical Institute, the Kenneth Rainin Foundation, the Crohns & & Colitis Foundation, and the Takeda-Columbia-NYU Alliance.
Dr. Koide has actually received research assistance from Argenx BVBA, Black Diamond Therapeutics, and Puretech Health, and has actually served as an expert for Black Diamond Therapeutics. NYU Langone has patents pending (10,722,600, 62/935,035, and 63/157,225) for therapies established from this treatment method, from which Dr. Cadwell, Dr. Koide, Dr. Matsuzawa-Ishimoto, and NYU Langone may benefit economically.
New research might have resolved a mystery surrounding Crohns disease, a type of inflammatory bowel illness where immune defenses suggested to attack invading microbes mistakenly target the bodys own digestive system rather. It is likewise one of a number of infections and bacteria thought to activate disease start in individuals with Crohns disease, however the field does not understand why.
The researchers also found that norovirus infection obstructs T cell secretion of API5 in mice bred to have a rodent type of Crohns disease, killing gut lining cells in the procedure.
In experiments centered on mice genetically modified to have the mutation connected to Crohns disease in human beings, mice that got an injection of API5 survived, while half of the untreated group passed away. In human tissue, the investigators discovered that those with Crohns disease had between 5- and 10-fold fewer API5-producing T cells in their gut tissue than those without the health problem.
Released on October 5, 2022, in the journal Nature, the new research in mice and in human tissue revealed for the very first time that in healthy individuals, immune defenders called T cells secrete a protein called apoptosis inhibitor 5 (API5), which signifies the body immune system to stop the attack on gut lining cells. This protein includes an additional layer of defense versus immune damage, so even those with the mutation can have a healthy gut. The scientists also found that norovirus infection obstructs T cell secretion of API5 in mice bred to have a rodent form of Crohns illness, eliminating gut lining cells in the procedure.
Led by researchers at NYU Grossman School of Medicine, the research findings support the theory that API5 safeguards many people with the mutation against the illness up until a second trigger, such as norovirus infection, presses some throughout the disease limit.
In experiments centered on mice genetically customized to have the mutation linked to Crohns disease in human beings, mice that received an injection of API5 made it through, while half of the neglected group passed away. This verified the hypothesis that the protein safeguards gut cells, state the research study authors. In human tissue, the detectives discovered that those with Crohns disease had in between 5- and 10-fold less API5-producing T cells in their gut tissue than those without the health problem.
” Our study suggests that when norovirus contaminates those with a deteriorated capability to produce apoptosis inhibitor 5, it suggestions the balance towards a full-blown autoimmune illness.”– Ken H. Cadwell, PhD
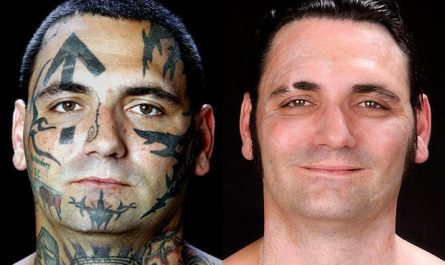
A mystery surrounding Crohns disease, a type of inflammatory bowel disease, may have been fixed by a new study. This image depicts an intestinal tract affected by Crohns disease.
New research might have resolved a secret surrounding Crohns disease, a kind of inflammatory bowel disease where immune defenses meant to assault getting into microorganisms mistakenly target the bodys own gastrointestinal tract instead. Norovirus is a common infection that causes throwing up and diarrhea. It is likewise among a number of infections and germs believed to set off illness start in individuals with Crohns illness, however the field does not know why.
” Our findings provide new insight into the crucial role that apoptosis inhibitor 5 plays in Crohns illness,” says Yu Matsuzawa-Ishimoto, MD, PhD, the research studys lead author and a gastroenterologist. “This molecule might offer a brand-new target for treating this persistent autoimmune illness, which has actually shown tough to handle over the long term.”
According to Dr. Matsuzawa-Ishimoto, a postdoctoral research fellow at NYU Langone Health, current treatments, which work by reducing the immune system, put patients at high danger for infection and typically end up being less reliable after a few years of use. A treatment technique targeting API5, he includes, may avoid those issues.
In another set of experiments, the private investigators created organ-like structures out of tissue gathered from human beings who tested favorable for the mutation. Especially, these structures were made only of gut-lining cells. Then, the research team dropped API5 into these “small guts” and discovered that this treatment secured gut lining cells. In addition, adding API5-producing T cells also secured the gut lining.
Norovirus is a very infectious infection that triggers vomiting and diarrhea. Anybody can get ill and infected with norovirus, and outbreaks are common. You might hear norovirus health problem be called “food poisoning,” “swallow bug,” or “stomach influenza.” Noroviruses are the leading cause of foodborne health problem, other germs and chemicals can likewise trigger foodborne disease.
When past research studies discovered that a specific hereditary change (mutation) is present in the majority of people with the condition, one clue emerged. This hereditary mutation makes gut lining cells more susceptible to damage. The mystery deepened once again when it was discovered that half of all Americans have this exact same risk-conferring hereditary anomaly, however less than half a million develop Crohns illness.