The group identified a brain network that prevails for all psychiatric health problems. This discovery opens new chances for future research study, such as looking at brain scans to see if the very same circuit is active and comparing distinctions between psychiatric disorders utilizing this circuit.
The study made use of several existing datasets to explore the neural basis of different psychiatric disorders and found a typical network for all of them.
Almost one in 5 grownups in the United States is affected by psychiatric conditions such as schizophrenia and anxiety. Additionally, about half of clients diagnosed with a psychiatric disease also have signs of another disorder. This overlap has led scientists to think that there might be a single neurobiological explanation for various psychiatric illnesses.
A group of researchers from Brigham and Womens Hospital, a member of the Mass General Brigham health care system, studied four existing psychiatric and neurological datasets and determined a network of brain locations underlying psychiatric illnesses. The outcomes of the research study were recently published in the journal Nature Human Behavior.
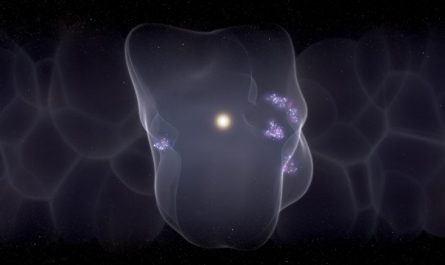
To resolve these drawbacks, the team utilized the human connectome (an electrical wiring diagram of the human brain) to evaluate whether gray matter modifications in psychiatric health problem more successfully mapped to a typical brain network than they did to common brain regions. The transdiagnostic network stayed robust, suggesting that no single psychiatric illness was disproportionately responsible for the network they recognized.
In subsequent analyses of a dataset consisting of brain imaging from 194 veterans with and without permeating head injury along with their psychiatric diagnoses, the researchers overlayed sores onto the transdiagnostic network and discovered that lesion-induced damage in the network correlated with a higher possibility of multiple psychiatric illnesses. They found that this lesion-based psychiatric network was really comparable to their atrophy-based psychiatric network in spite of having been derived from an entirely various dataset.
“We discovered that sores to those areas were associated with less psychiatric health problem, not more, so atrophy in that cingulate and insula might be a consequence or a compensation for psychiatric illness rather than a cause of it,” said Taylor.
” Traditionally, neurology and psychiatry have various diagnostic strategies,” said corresponding author Joseph J. Taylor, MD, Ph.D., Medical Director of Transcranial Magnetic Stimulation at the Brighams Center for Brain Circuit Therapeutics and an associate psychiatrist in the Brighams Department of Psychiatry.
We now have tools to explore the where concern for psychiatry disorders. In this study, we examined whether psychiatric conditions share a typical brain network.”
The scientists started by evaluating a set of structural brain information from over 15,000 healthy controls as well as patients detected with schizophrenia, bipolar condition, depression, addiction, obsessive-compulsive condition, or anxiety. They discovered gray matter reduces in anterior cingulate and insula, two brain areas typically associated with psychiatric illness.
To address these imperfections, the group utilized the human connectome (a circuitry diagram of the human brain) to evaluate whether noodle changes in psychiatric disease better mapped to a common brain network than they did to common brain areas. The scientists discovered a transdiagnostic network in which up to 85 percent of studies revealed gray matter decreases. This network was particular to noodle decreases in psychiatric versus neurodegenerative disorders. They then carried out the very same analyses while neglecting data from one psychiatric medical diagnosis at a time. The transdiagnostic network stayed robust, suggesting that no single psychiatric illness was disproportionately responsible for the network they recognized.
In subsequent analyses of a dataset consisting of brain imaging from 194 veterans with and without permeating head injury along with their psychiatric medical diagnoses, the scientists overlayed lesions onto the transdiagnostic network and discovered that lesion-induced damage in the network correlated with a greater possibility of multiple psychiatric diseases. They also utilized the veteran information to independently obtain a transdiagnostic network based upon brain lesions related to psychiatric disease. They discovered that this lesion-based psychiatric network was extremely comparable to their atrophy-based psychiatric network despite having been derived from a totally different dataset.
The team utilized data from neurosurgical ablations for patients with otherwise untreatable and severe psychiatric health problems. These ablation targets aligned with the transdiagnostic network.
The majority of remarkably, said Taylor, their findings appear to challenge the concept that noodle decreases in the anterior cingulate and insula are causally associated with psychiatric disease. “We found that sores to those regions were associated with less psychiatric illness, not more, so atrophy in that cingulate and insula may be a repercussion or a compensation for psychiatric disease instead of a reason for it,” said Taylor. Rather, their analyses indicate the posterior parietal cortex as the brain network node probably to be causally connected with psychiatric illness.
By recognizing a significant, delicate, and specific transdiagnostic network for psychiatric disease, the group has actually opened up a number of possible new instructions for follow-up studies, including analyzing existing fMRI datasets to see if neural activation patterns follow the very same circuit and examining circuit-based differences across psychiatric disorders. Taylor also intends on using Transcranial Magnetic Stimulation (TMS) to regulate the network, specifically using the posterior parietal area as a target.
” Psychiatric conditions are brain conditions, and now were just beginning to have the tools to study and modulate their underlying circuitry,” stated Taylor. “There might be more in typical across these conditions than we initially believed.”
Referral: “A transdiagnostic network for psychiatric health problem originated from atrophy and sores” by Joseph J. Taylor, Christopher Lin, Daniel Talmasov, Michael A. Ferguson, Frederic L. W. V. J. Schaper, Jing Jiang, Madeleine Goodkind, Jordan Grafman, Amit Etkin, Shan H. Siddiqi, and Michael D. Fox, 12 January 2023, Nature Human Behaviour.DOI: 10.1038/ s41562-022-01501-9.
SS: Owner of intellectual property involving the use of brain connectivity to target TMS, scientific expert for Magnus Medical, investigator-initiated research study financing from Neuronetics and Brainsway, speaking costs from Brainsway and Otsuka (for PsychU.org), shareholder in Brainsway (publicly traded) and Magnus Medical (not publicly traded). MDF: Scientific expert for Magnus Medical, owns independent intellectual home involving the usage of functional connection to target TMS. This intellectual residential or commercial property was not utilized in the present manuscript.