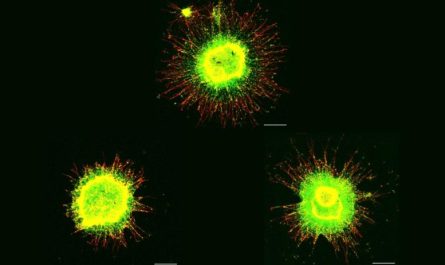
A research study group at LKS Faculty of Medicine, The University of Hong Kong (HKUMed) discovered that exosomes derived from γδ-T cells (γδ-T-Exos) synergised with radiotherapy can control nasopharyngeal cancer (NPC) by getting rid of the radioresistance of NPC cancer stem cells (CSCs) and maintain their tumor-killing and T cell-promoting activities in the immunosuppressive NPC microenvironment. Herein, the research team found that γδ-T-Exos not just successfully communicated with NPC cells and induced tumor cell death in vitro, which was mainly moderated by Fas/Fas ligand (FasL) and death receptor 5 (DR5)/ tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) paths, but likewise managed NPC tumor development and prolonged tumor-bearing mice survival in vivo. The combination of γδ-T-Exos with radiotherapy overcame the radioresistance of CD44+/ high NPC cells and significantly improved its therapeutic efficacy versus NPC in vitro and in vivo. In addition, γδ-T-Exos promoted T-cell migration into NPC tumors by upregulating CCR5 on T cells that were chemoattracted by CCR5 ligands in the NPC growth microenvironment. NPC growth cells secreted plentiful tumor growth aspect beta (TGF-β) to suppress T- cell responses, γδ-T-Exos protected their direct anti-tumor activities and overcame the immunosuppressive NPC microenvironment to amplify T-cell anti-tumor resistance.
Background
Nasopharyngeal carcinoma (NPC) is among the most aggressive Epstein-Barr virus (EBV)- related growths and is very widespread in East Asia, consisting of Hong Kong Radiotherapy is the first-line treatment for NPC, its therapeutic performance is limited in some patients due to radioresistance. Adoptive T cell immunotherapy has also shown guarantee in the treatment of NPC; however, its anti-tumor efficiency might be hampered by an immunosuppressive tumor microenvironment. Exosomes are microscopic extracellular vesicles that originate in the endosome and promote intercellular interaction. Cell-free exosomes provide higher safety, simpler storage, and cheaper expenses than cell-based treatment. Scientist formerly established that γδ-T-Exos may effectively limit the progression of EBV-associated growths in a previous study. It stays unidentified whether γδ-T-Exos have a synergistic result with radiotherapy and maintain their anti-tumor activities versus NPC in an immunosuppressive tumor microenvironment.
HKUMed establishes an unique restorative approach versus nasopharyngeal carcinoma by utilizing exosomes stemmed from γδ-T cells synergize with radiotherapy. The research study was led by Professor Tu Wenwei, Department of Paediatrics and Adolescent Medicine, School of Clinical Medicine, HKUMed (middle), and Dr. Wang Xiwei, post-doctoral fellow of Professor Tus team (left), is the first author. PhD student Zhang Yanmei (best) belongs to the research study group. Credit: The University of Hong Kong.
Research findings
Herein, the research study group found that γδ-T-Exos not just efficiently interacted with NPC cells and caused tumor cell death in vitro, which was generally moderated by Fas/Fas ligand (FasL) and death receptor 5 (DR5)/ growth necrosis factor-related apoptosis-inducing ligand (TRAIL) pathways, but likewise controlled NPC tumor growth and extended tumor-bearing mice survival in vivo. Moreover, γδ-T-Exos selectively targeted the radioresistant CD44+/ high CSCs and caused profound cell apoptosis. The combination of γδ-T-Exos with radiotherapy conquered the radioresistance of CD44+/ high NPC cells and substantially enhanced its healing efficacy versus NPC in vitro and in vivo. In addition, γδ-T-Exos promoted T-cell migration into NPC growths by upregulating CCR5 on T cells that were chemoattracted by CCR5 ligands in the NPC growth microenvironment. NPC growth cells secreted abundant tumor growth element beta (TGF-β) to suppress T- cell responses, γδ-T-Exos maintained their direct anti-tumor activities and overcame the immunosuppressive NPC microenvironment to magnify T-cell anti-tumor immunity.
Our study initially offers a strong pre-clinical proof of concept utilizing a novel therapeutic method by combining γδ-T-Exos with radiotherapy to deal with NPC. γδ-T-Exos can effectively connect with and eliminate both EBV unfavorable and favorable NPC cells. More notably, γδ-T-Exos can eradicate radioresistant NPC CSCs and preserve their tumor-killing and T cell-promoting activities in the immunosuppressive NPC microenvironment. Mix of radiotherapy with γδ-T- Exos has fantastic prospective in the treatment of NPC, which will be highly advantageous to the clinical application of this technique, stated Professor Tu Wenwei of the Department of Paediatrics and Adolescent Medicine, School of Clinical Medicine, HKUMed, who led the research.
Significance of the research study
The findings of the study have considerable ramifications in cancer immunotherapy. Firstly, γδ-T-Exos engaged with CD44+/ high NPC CSCs in high efficacy. For that reason, γδ-T-Exos can supplement radiotherapy and improve its therapeutic effectiveness against NPC. γδ-T-Exos has advantages over other exosome-based therapies in combination with ionizing irradiation in NPC treatment (e.g. MSC-Exos) by protecting anti-tumor activities in the immunosuppressive NPC microenvironment and are easier in preparation. The outcomes that γδ-T-Exos broadened pre-existing tumor-specific T cells in the immunosuppressive NPC microenvironment can considerably improve the medical feasibility of γδ-T-Exos. Therefore, it is very important for the mix treatment to have immunostimulatory impacts to boost anti-tumor immunity in the immunosuppressive NPC microenvironment.
The research was led by Professor Tu Wenwei, Department of Paediatrics and Adolescent Medicine, School of Clinical Medicine, HKUMed. Credit: The University of Hong Kong
About the research study group
The research study was led by Professor Tu Wenwei, Department of Paediatrics and Adolescent Medicine, School of Clinical Medicine, HKUMed. Dr. Wang Xiwei, post-doctoral fellow of Professor Tus group, is the very first author. Other scientists consist of Ms. Zhang Yanmei, PhD student; Dr. Mu Xiaofeng, post-doctoral fellow and Ms. Chung Yuet, Research Assistant of Professor Tus group; Ms. Chloe Tu Ran, Computational and Systems Biology Interdepartmental Program, University of California, Los Angeles, California, the United States. Teacher George Tsao Sai-wah, Principal Lecturer, School of Biomedical Sciences, HKUMed. Teacher Godfrey Chan Chi-fung, Tsao Yen-Chow Professor in Paediatrics and Adolescent Medicine, Clinical Professor of Paediatrics and Adolescent Medicine, HKUMed; Professor Leung Wing-hang, Chairperson and Clinical Professor, Department of Paediatrics and Adolescent Medicine, School for Clinical Medicine, HKUMed; Professor Lau Yu-lung, Doris Zimmern Professor in Community Child Health and Chair Professor of Paediatrics, Department of Paediatrics and Adolescent Medicine, School for Clinical Medicine, HKUMed; Dr. Liu Yinping, Research Officer, Department of Paediatrics and Adolescent Medicine, School for Clinical Medicine, HKUMed.
The Institute of Computational and Systems Biology Interdepartmental Program, University of California, Los Angeles, California, USA likewise contributed to this research study.
Recommendations
This work was supported in part by Health and Medical Research Fund, Food and Health Bureau, Hong Kong SAR Government (18192021); Strategic Interdisciplinary Research Scheme, University of Hong Kong; General Research Fund (17122519, 17126317, 17114818, 17122420 and 17104617) from Research Grants Council, University Grants Committee, Government of the Hong Kong Special Administrative Region.
Referral: “Exosomes originated from γδ-T cells synergize with radiotherapy and preserve antitumor activities against nasopharyngeal cancer in immunosuppressive microenvironment” by Xiwei Wang, Yanmei Zhang, Xiaofeng Mu, Chloe Ran Tu, Yuet Chung, Sai Wah Tsao, Godfrey Chi-Fung Chan, Wing-Hang Leung, Yu-lung Lau, Yinping Liu and Wenwei Tu, February 2022, Journal for Immunotherapy of Cancer.DOI: 10.1136/ jitc-2021-003832.
HKUMed establishes a novel healing method versus nasopharyngeal carcinoma by utilizing exosomes obtained from γδ-T cells synergized with radiotherapy
A research study team at LKS Faculty of Medicine, The University of Hong Kong (HKUMed) discovered that exosomes originated from γδ-T cells (γδ-T-Exos) synergised with radiotherapy can control nasopharyngeal cancer (NPC) by conquering the radioresistance of NPC cancer stem cells (CSCs) and preserve their tumor-killing and T cell-promoting activities in the immunosuppressive NPC microenvironment. This research study supplies an evidence of concept for a novel and powerful technique by integrating γδ-T-Exos with radiotherapy in the control of NPC. The groundbreaking research study was published in the distinguished academic journal Journal of Immunotherapy of Cancer.