This is the first research study to effectively measure the result of ultrasound-based blood-brain barrier opening on the concentrations of chemotherapy in the human brain. Opening the blood-brain barrier led to an approximately 4- to six-fold increase in drug concentrations in the human brain, the results showed.
Scientists observed this boost with two different effective chemotherapy drugs, paclitaxel, and carboplatin. The drugs are not used to deal with these clients because they do not cross the blood-brain barrier in typical situations.
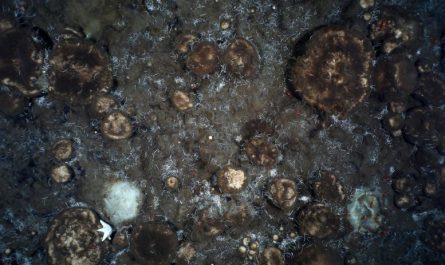
Following brain sonication and administration of intravenous microbubbles, scientists injected fluorescein intravenously, as this color does not generally penetrate into the brain. They first observed fluorescein in the arteries, then the whole brain was fluorescent, as this color was in the capillaries, followed by the brain veins.
In addition, this is the first study to explain how quickly the blood-brain barrier closes after sonication. Most of the blood-brain barrier repair takes place in the first 30 to 60 minutes after sonication, the researchers discovered. The findings will allow optimization of the series of drug delivery and ultrasound activation to maximize the drug penetration into the human brain, the authors stated.
” This is potentially a substantial advance for glioblastoma patients,” said lead detective Dr. Adam Sonabend, an associate professor of neurological surgical treatment at Northwestern University Feinberg School of Medicine and a Northwestern Medicine neurosurgeon.
Temozolomide, the current chemotherapy used for glioblastoma, does cross the blood-brain barrier, however is a weak drug, Sonabend stated.
The paper was current released in the journal The Lancet Oncology.
Patients with brain cancer can not be treated with most drugs that are otherwise effective for cancer elsewhere in the body, as these do not cross the blood-brain barrier. Reliable repurposing of drugs to treat brain pathology and cancer needs their delivery to the brain.
In the past, research studies that injected paclitaxel directly into the brain of clients with these growths observed appealing indications of effectiveness, but the direct injection was connected with toxicity such as brain irritation and meningitis, Sonabend stated.
Blood-brain barrier recloses after an hour
The researchers found that making use of ultrasound and microbubble-based opening of the blood-brain barrier is transient, and the majority of the blood-brain barrier stability is restored within one hour after this treatment in human beings.
” There is a vital time window after sonification when the brain is permeable to drugs flowing in the blood stream,” Sonabend stated.
Previous human studies revealed that the blood-brain barrier is completely restored 24 hours after brain sonication, and based upon some animal studies, the field assumed that the blood-brain barrier is open for the first 6 hours approximately. The Northwestern study reveals that this time window might be much shorter.
In another first, the study reports that utilizing a novel skull-implantable grid of 9 ultrasound emitters created by French biotech business Carthera opens the blood-brain barrier in a volume of brain that is nine times bigger than the preliminary device (a small single-ultrasound emitter implant). This is essential due to the fact that to be efficient, this technique requires coverage of a big area of the brain adjacent to the cavity that stays in the brain after the elimination of glioblastoma growths.
Scientific trial for patients with frequent glioblastoma
The findings of the research study are the basis for an ongoing stage 2 scientific trial the scientists are conducting for clients with frequent glioblastoma. The goal of the trial– in which individuals get a combination of paclitaxel and carboplatin delivered to their brain with the ultrasound strategy– is to investigate whether this treatment lengthens the survival of these clients. A mix of these two drugs is utilized in other cancers, which is the basis for combining them in the phase 2 trial.
In the phase 1 medical trial reported in this paper, patients underwent surgery for resection of their tumors and implantation of the ultrasound device. They began treatment within a few weeks after the implantation.
Scientists intensified the dosage of paclitaxel provided every 3 weeks with the accompanying ultrasound-based blood-brain barrier opening. In subsets of clients, research studies were carried out throughout surgery to investigate the result of this ultrasound device on drug concentrations. The blood-brain barrier was imagined and mapped in the operating room using a fluorescent die called fluorescein and by MRI obtained after ultrasound therapy.
” While we have concentrated on brain cancer (for which there are approximately 30,000 gliomas in the U.S.), this unlocks to investigate unique drug-based treatments for countless patients who experience different brain illness,” Sonabend stated.
Referral: “Repeated blood– brain barrier opening with an implantable ultrasound device for shipment of albumin-bound paclitaxel in patients with frequent glioblastoma: a phase 1 trial” by Adam M Sonabend, Andrew Gould, Christina Amidei, Rachel Ward, Karyn A Schmidt, Daniel Y Zhang, Cristal Gomez, John F Bebawy, Benjamin P Liu, Guillaume Bouchoux, Carole Desseaux, Irene B Helenowski, Rimas V Lukas, Karan Dixit, Priya Kumthekar, Víctor A Arrieta, Maciej S Lesniak, Alexandre Carpentier, Hui Zhang, Miguel Muzzio and Roger Stupp, 2 May 2023, The Lancet Oncology.DOI: 10.1016/ S1470-2045( 23 )00112-2.
The study was funded by the National Cancer Institute.
The very first human trial of a novel ultrasound gadget showed its prospective to briefly provide and open the blood-brain barrier chemotherapy straight to the brain. This innovative treatment resulted in a substantial boost of 4 to 6 times in drug concentrations in the brain, and clients were awake throughout the four-minute treatment which was repeated every couple of weeks for several months. Currently, there is no effective treatment for glioblastoma, making this new ultrasound method a promising development in the fight versus this ravaging illness.
An unique ultrasound technique making use of microbubbles momentarily opens the blood-brain barrier to treat glioblastoma in people.
One of the biggest obstacles in dealing with glioblastoma, a fatal brain cancer, is that the most efficient chemotherapy drugs can not penetrate the blood-brain barrier to reach the fast-growing brain growth.
Northwestern Medicine scientists have actually recently reported the outcomes of the first human scientific trial where they utilized a new, skull-implantable ultrasound device. This gadget opens the blood-brain barrier, permitting for repeated permeation of big areas of the brain, therefore enabling the delivery of intravenously injected chemotherapy.
The four-minute procedure to open the blood-brain barrier is performed with the patient awake, and clients go home after a few hours. The results reveal the treatment is safe and well tolerated, with some clients getting up to six cycles of treatment.
Following brain sonication and administration of intravenous microbubbles, researchers injected fluorescein intravenously, as this dye does not normally permeate into the brain. They first observed fluorescein in the arteries, then the whole brain was fluorescent, as this color was in the blood vessels, followed by the brain veins. The blood-brain barrier is a tiny structure that shields the brain from the huge majority of circulating drugs. Patients with brain cancer can not be treated with most drugs that are otherwise reliable for cancer in other places in the body, as these do not cross the blood-brain barrier. Effective repurposing of drugs to deal with brain pathology and cancer requires their delivery to the brain.