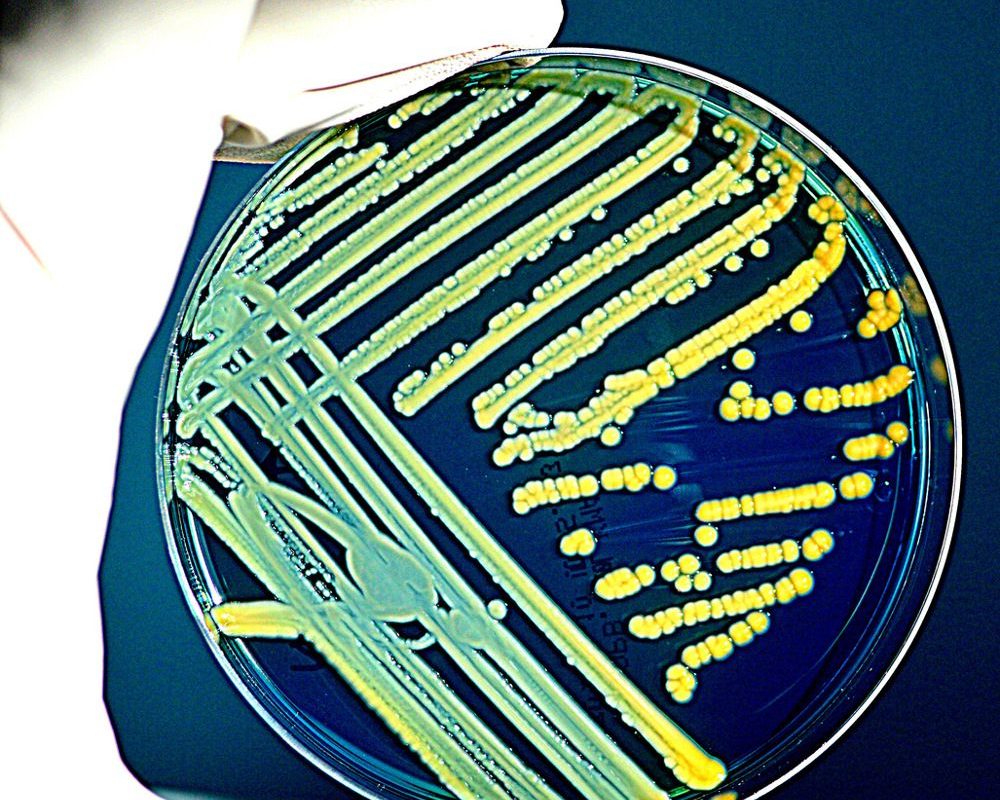
The guts natural occupants are crucial to preventing and fighting some infections. Take Clostridioides difficile, a germs causing serious diarrhea that can be life-threatening: it is most likely to trigger infection in a gut with a modified microbiota, often due to antibiotic treatment. On the other hand, fecal microbiota transplants from healthy donors have actually proven useful to treat the disease, additional proof for the role of commensal bacteria in fending off the infection. How commensals combat versus such pathogens is beginning to come into focus. Warfare– through poisonous substances or other weapons– and competition for resources are two common methods. Now, a trio of studies released this month provides insight into how specific commensals might keep the gut safe from colonization by pathogens using these strategies. Together, the findings hold promise for the future design and prescription of probiotics to assist fend off transmittable diseases. Vibrio cholerae: When your weapons are unsatisfactory Together with her colleagues, Melanie Blokesch, a microbiologist at the Swiss Federal Institute of Technology in Lausanne, had revealed in recent years that Vibrio cholerae, the germs responsible for cholera, releases a killing device when it grows on chitin– a polymer that comprises shellfish exoskeletons. Chitinous surface areas are abundant in the Bay of Bengal to the southeast of India, and cholera is endemic in seaside villages of the nation and neighboring Bangladesh. The killing device, referred to as the type VI secretion system (T6SS), is a sort of molecular spear utilized by V. cholerae and numerous other germs to inject toxins into neighboring cells. On chitinous surfaces, says Blokesch, the T6SS is upregulated, making this pathogen “prepared to eliminate other germs once people consume them [from] contaminated water.” Vibrio choleraeHer group has actually generally studied V. choleraes way of life outside the body and on natural surface areas, and she states she wished to understand what takes place when the pathogen gets into human beings– that is, whether resident microorganisms in the gut would yield or endure to V. choleraes T6SS weapon. Using 26 bacterial isolates from the Human Gastrointestinal Bacteria Culture Collection– made from samples from healthy people– the scientists had each of these strains take on against V. cholerae in a meal. A few of these commensals lost the fight versus the pathogen, however a few endured. Enterobacter cloacae was among the survivors. Not just did it endure the conflict, but Blokesch and her colleagues found that it really eliminated V. cholerae. The key to the species success is that it has its own, remarkable T6SS– E. cloacae mutants with an inactive weapon proved defenseless against the pathogen. Yet what made E. cloacaes T6SS much better than V. choleraes is uncertain. Other survivors of the microbial faceoff were members of the Klebsiella genus, consisting of K. michiganensis and K. oxytoca. They did not kill V. cholerae, but rather produced a polysaccharide that is anchored to Klebsiella germss membranes, making a guard. Understood as pill group I, these sugary coats saved the microorganisms from V. choleraes T6SS attacks. If bacteria produced this specific capsule group, they had a much better possibility of surviving the battle with V. cholerae– a finding that is quite robust, states Benjamin Ross, a microbiologist at the Geisel School of Medicine at Dartmouth who was not included in the study. Karina Xavier, a molecular biologist at the Instituto Gulbenkian de Ciência in Portugal who also did not get involved in the research study, speculates that, because they endure such attacks, Klebsiella species might be able to protect their hosts by taking on V. cholerae for resources. Many Klebsiella strains efficiently consume different types of nutrients, and as other recent studies have discovered, harboring gut germs that are great at consuming resources can be vital for withstanding pathogenic infection. See “Probiotics Prevent Cholera in Animal Models” Salmonella Typhimurium: When the leftovers are goneBärbel Stecher, a microbiologist at Ludwig Maximilian University of Munich, has for a very long time studied how mammalian gut microbiota provide colonization resistance against Salmonella enterica serovar Typhimurium (S. Tm), one of the leading causes of food poisoning. A couple of years earlier, she and her associates developed a synthetic murine bacterial community including 12 types that, when transplanted into the gut of a germ-free mouse, provided partial resistance against Salmonella infection. They later discovered that when they included an E. coli pressure to the mix, the mice were completely secured– similar to what a far more complicated microbiome does, she says. Escherichia coliE. coli is “of essential value for the colonization resistance” in this design, notes Stecher. But she and her associates observed that its existence might just secure mice from a Salmonella infection when the rest of their microbial neighborhood had a specific structure; mice whose microbiota consisted of only 3 species caught Salmonella even when inoculated with the very same E. coli pressure. The system behind this difference in outcomes was uncertain, so Stechers group looked into the genes revealed by E. coli in mice with more- and less-diverse microbiomes. The analysis revealed that the majority of genes that were differentially regulated in E. coli under the two conditions were associated with carbohydrate metabolic process. “This recommended that they simply have more carbohydrates offered under one condition versus the other,” states Stecher. By additional digging into the contextual differences, the team found that in the 12-species microbiota, E. coli and S. Tm seemed to be contending for galactitol, a sugar that none of the other 12 commensal types takes in, which this competitors was essential to avoiding infection in the mice. In the less complicated three-species community, E. coli did not deplete galactitol, rather utilizing other basic sugars that in the previous circumstance were made use of by other members of the microbiota, specifically those belonging to the family Lachnospiraceae. The main takeaway from these outcomes, according to Mariana Byndloss, a microbiologist at Vanderbilt University Medical Center who peer evaluated the study, is “that commensal germs protect the host from pathogens by completing for nutrients.” Byndloss includes that as the study used a synthetic neighborhood of microorganisms in a mouse model, “we do not know if this competition is happening in the human gut. [It will be] important to eventually equate those findings from animal models into people.” See “Gut Microbes Help Coordinate Immune Activity in Mice” Klebsiella pneumoniae: When a close relative is better at the tableTill Strowig, a microbiologist at the Helmholtz Centre for Infection Research in Germany, and his colleagues found that resource competition was likewise key to colonization resistance against another feared pathogen: Klebsiella pneumoniae, which in recent years has been extensively related to hospital-acquired infections by multidrug-resistant stress. See “Gut Microbe Linked to Nonalcoholic Fatty Liver Disease” Their method was initially different from that of Stechers team. Strowig and associates gathered fecal samples from healthy adults and kids, nurtured them with a multidrug resistant pressure of K. pneumoniae, and waited to see whether the pathogen might make it through after experiencing the diverse microbiomes in these fresh feces. Strowig says he anticipated that their microbiomes would not be susceptible to the pathogen, however surprisingly, a lot of them were. The ability of these samples to withstand K. pneumoniae colonization was, in reality, strikingly variable. “There was a 100,000-fold distinction between individuals,” he says, “and that caught our interest.” The team discovered that a number of the samples that were most resistant to K. pneumoniae– especially those acquired from kids– had a common species: Klebsiella oxytoca. To explore the prospective protective power of this commensal, the team offered it to mice with a microbiota formerly interfered with by antibiotics and evaluated whether its presence could prevent a K. pneumoniae infection. Klebsiella pneumoniaeIt ended up that certainly, mice treated with K. oxytoca were secured. Not only did the types avoid colonization by K. pneumoniae, it also cleared the pathogen in experiments where K. pneumoniae was presented at the exact same time or prior to K. oxytoca shot. Similar to the protection E. coli used versus Salmonella infection, K. oxytocas success turned out to arise from competition for using a particular carbon source– in this case, beta-glucosides. Strowig and his coworkers discovered that the commensal has genes included in the metabolic process of beta-glucosidic sugars, and the group ended up being especially interested in an aspect present in all K. oxytoca protective stress but missing in K. pneumoniae: the casRAB operon, which includes casA, the gene for a protein that transports beta-glucosidic sugars into the cell. In more experiments, the group discovered that casA undoubtedly seems type in the competition: K. oxytoca doing not have the gene was unable to prevent the pathogenic colonization. K. pneumoniae does not have casA in its genome, it does appear to take in beta-glucosidic sugars, states Strowig, likely using other transporters to do so. The groups hypothesis, he adds, is that the protein encoded by casA is particularly effective in transporting beta-glucosidic sugars into cells, allowing K. oxytoca to outcompete its pathogenic relative. Similar to E. colis competitors with Salmonella, the study authors found that other strains in the microbiota contributed to K. oxytocas success in restricting K. pneumoniae, most likely by depleting specific resources. Xavier, who peer-reviewed Stechers paper but was not involved in that research study or in Strowigs, says that findings presented in both papers provide “a description for why various individuals have different vulnerabilities” to these pathogens. That is, she states, it may depend on whether protective pressures of commensal microorganisms exist.” I think one can hope or imagine that for each pathogen there may be a commensal [bacterial strain] with a high metabolic overlap” to outcompete it– and finding those competitive opponents could be an appealing technique for developing new probiotics. “We require to profit from the incredible capacity of these commensal microorganisms and their protective capabilities.” Probiotics: A promising path to treat infectionsMembers of the Klebsiella genus are one appealing option for the advancement of brand-new probiotics, says Xavier. In 2015, her team reported that the commensal Klebsiella michiganensis supplied colonization resistance versus an attacking E. coli and Salmonella through nutrient competitors. The brand-new findings from groups led by Blokesch and Strowig additional support this genuss potential. Both Xavier and Strowig warn that the development of probiotics with Klebsiella species ought to be resolved carefully, given the pathogenic nature of some stress and their capability to acquire antibiotic resistance through horizontal gene transfer. “We dont want to have a probiotic that has too much pathogenic capacity,” Strowig says. The goal, he adds, is to make a stress that is safe without compromising its protective residential or commercial properties. The University of Oxfords Emily Stevens, who studies the function of host microbiota in the evolution of pathogens, concurs. “Both the microbiota and the pathogen have the capability to progress in response to the actions of the other,” she states; as such, scientists must think about “how any microbes that you offer to a host may communicate with any resident microbiota, whether any of these microorganisms have the potential in one form or another to trigger illness, [and] whether they may drive evolutionary modifications in the pathogen.” In the light of the existing crisis of widespread antibiotic resistance in pathogens, “there is a real pushing requirement to discover options” for treating infections, says Stevens. The development of microbiota-based therapies, she includes, “is a actually interesting and promising potential option.” See “Gut Microbiome May Help or Hinder Defenses Against SARS-CoV-2”
Other survivors of the microbial faceoff were members of the Klebsiella genus, including K. michiganensis and K. oxytoca. Strowig and coworkers gathered fecal samples from healthy grownups and kids, bred them with a multidrug resistant strain of K. pneumoniae, and waited to see whether the pathogen might survive after encountering the varied microbiomes in these fresh feces. To explore the potential protective power of this commensal, the group provided it to mice with a microbiota formerly disrupted by prescription antibiotics and evaluated whether its existence might avoid a K. pneumoniae infection. Strowig and his associates found that the commensal has genes involved in the metabolism of beta-glucosidic sugars, and the group became especially interested in an element present in all K. oxytoca protective pressures however missing in K. pneumoniae: the casRAB operon, which consists of casA, the gene for a protein that transfers beta-glucosidic sugars into the cell. K. pneumoniae does not have casA in its genome, it does appear to consume beta-glucosidic sugars, states Strowig, most likely using other transporters to do so.