Schizophrenia client samples had actually lowered expression of two genes vital for brain advancement, a regulator of gene expression called BRN2 and a cell development promoter called pleiotrophin. Replacing the missing out on BRN2 in the cells restored brain cell production, while including pleiotrophin reduced brain cell death. If more research studies validate these results, it might lead to the advancement of targeted therapies that assist correct these genetic distinctions in particular brain cell types.
They are focusing on the function of endothelial cells, cells that normally line the blood vessels and release important immune molecules called cytokines.
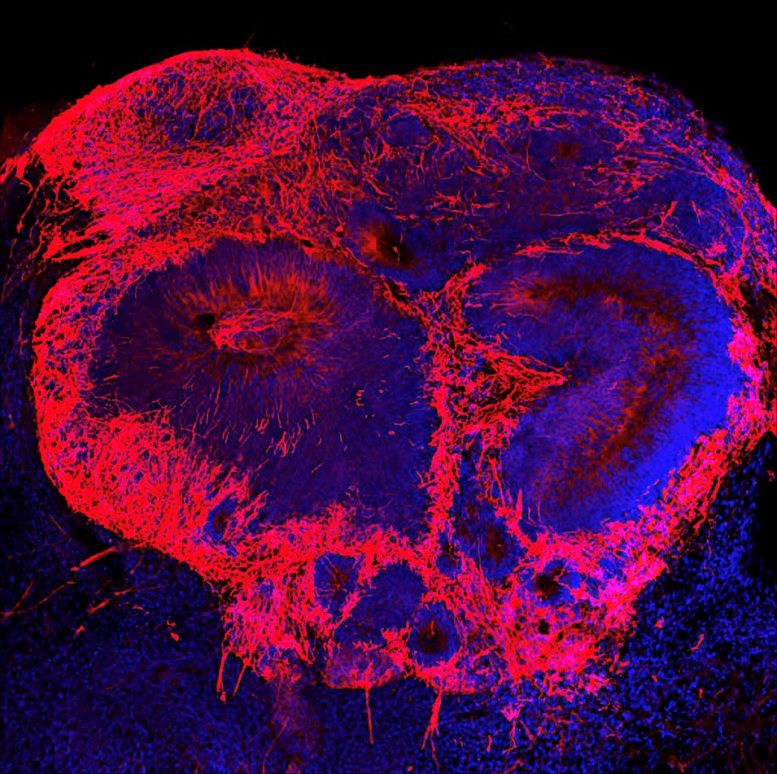
Increasing levels of a possible disease aspect leads to extra brain cells (red) in a schizophrenia brain organoid. Credit: Image courtesy of Dr. Michael Notaras
Multiple changes in brain cells during the first month of embryonic advancement may contribute to schizophrenia later on in life, according to a brand-new research study by Weill Cornell Medicine investigators.
The researchers, whose research study was published in Molecular Psychiatry, used stem cells collected from clients with schizophrenia and individuals without the illness to grow 3-dimensional “mini-brains” or organoids in the laboratory. By comparing the advancement of both sets of organoids, they found that a decreased expression of 2 genes in the cells stymies early advancement and triggers a scarcity of brain cells in organoids grown from patient stem cells.
” This discovery fills a crucial gap in researchers understanding of schizophrenia,” stated senior author Dr. Dilek Colak, assistant professor of neuroscience at the Feil Family Brain and Mind Institute and the Center for Neurogenetics at Weill Cornell Medicine. Symptoms of schizophrenia generally establish in adulthood, but postmortem studies of the brains of people with the illness discovered enlarged cavities called ventricles and differences in the cortical layers that likely took place early in life.
” There were tips schizophrenia began throughout early development, however we didnt have proof,” Dr. Colak stated.
By growing organoids from stem cells gathered from up to 21 human stem cell donors, the group, led by first author Dr. Michael Notaras, a previous NHMRC CJ Martin Fellow in Dr. Colaks laboratory, had the ability to grow brain tissue with each patients exact genetic make-up. They utilized single-cell RNA sequencing to compare gene expression in individual cells in clients tissue and in tissue grown from people without schizophrenia.
” We found a typical pathology among all the patients with schizophrenia regardless of each of the patients having distinct illness discussions,” Dr. Colak stated.
Schizophrenia client samples had actually lowered expression of 2 genes important for brain advancement, a regulator of gene expression called BRN2 and a cell growth promoter called pleiotrophin. Replacing the missing BRN2 in the cells brought back brain cell production, while adding pleiotrophin minimized brain cell death.
” Weve made a fundamental discovery offering what we think is the very first evidence in human tissue that multiple cell-specific systems exist and most likely contribute to risk of schizophrenia,” stated Dr. Notaras. “This forces us, as a field, to reconsider when illness truly starts and how we ought to think of establishing the next generation of schizophrenia rehabs.”
Dr. Colak and her coworkers are presently using the mini-brains to begin to tease out the function of private cell types and to better comprehend how genetic factors might engage with the environment to cause schizophrenia. They are focusing on the function of endothelial cells, cells that typically line the capillary and release crucial immune particles called cytokines. The mini-brains grown from patients with schizophrenia had an excess of early endothelial-related cells, which might lead to an excessive immune reaction to infection.
” This may describe the link in between maternal infections during pregnancy and schizophrenia seen in mouse research studies,” Dr. Colak stated.
In addition to helping researchers better comprehend schizophrenia, Dr. Colak said she thinks that mini-brains grown from clients stem cells may be a helpful tool for studying other brain diseases.
” The method could be used to study the early life pathology of late-onset neuropsychiatric or neurodegenerative illness like Alzheimers disease or Huntington disease,” Dr. Colak said.
Reference: “Schizophrenia is specified by cell-specific neuropathology and numerous neurodevelopmental mechanisms in patient-derived cerebral organoids” by Michael Notaras, Aiman Lodhi, Friederike Dündar, Paul Collier, Nicole M. Sayles, Hagen Tilgner, David Greening and Dilek Colak, 17 November 2021, Molecular Psychiatry.DOI: 10.1038/ s41380-021-01316-6.