The patient volunteers in the brand-new analysis belong to a larger, continuous research study based at Fred Hutch, the Seattle COVID Cohort Study, which is led by Julie McElrath, M.D., Ph.D., Senior Vice President and Director of Fred Hutchs Vaccine and Infectious Disease Division, and Julie Czartoski, ARNP, Research Clinician at the Hutch.
Flowing serum proteins 60 days after start of SARS-CoV-2 infectious symptoms determine a sub-category of long-COVID with relentless swelling. This signature assists clarify biological variety in long-COVID highlighting the requirement for targeted treatment techniques and reveals diagnostic utility for separating inflammatory and non-inflammatory long-COVID. Credit: Rachel Tompa, Ph.D./ Allen Institute
Researchers have seen previous links in between inflammation and long COVID, but the new research study is the very first to trace the persistence of these inflammatory markers over time in the same patients.
Theres an obvious implication to these findings, stated Troy Torgerson, M.D., Ph.D., Director of Experimental Immunology at the Allen Institute for Immunology, a division of the Allen Institute: Certain kinds of anti-inflammatory drugs may reduce signs for some long COVID patients. Physicians need a way of informing which long COVID patients may benefit from which treatment– a form of accuracy medication for a disease that so far remains maddeningly strange.
” The huge question was, can we specify which long COVID patients have persistent inflammation vs. those that do not? That would be useful in terms of scientific trial planning and in regards to assisting clinicians find out targeted treatments for their clients,” said Torgerson, who led the Nature Communications publication together with McElrath, Aarthi Talla, Senior Bioinformatician at the Allen Institute for Immunology, Suhas Vasaikar, Ph.D., former Senior Bioinformatics Scientist (now a Principal Scientist at Seagen), and Tom Bumol, Ph.D., previous Executive Vice President and Director.
Specifically, the blood markers uncovered in this subset of clients with “inflammatory long COVID,” as the researchers call it, indicate a flavor of swelling similar to that seen in autoimmune illness like rheumatoid arthritis. This sort of swelling can be treated with an existing class of drugs called JAK inhibitors, a minimum of in the case of rheumatoid arthritis (it has not yet been evaluated for long COVID).
The scientists also want to narrow down their molecular signature of “inflammatory long COVID” to a few markers that could be utilized in the clinic to arrange this subset of long COVID clients out from the rest.
Refining treatment alternatives
Launched in the spring of 2020, quickly after the COVID-19 pandemic closed down services and schools in the U.S., the Fred Hutch-led Seattle COVID Cohort Study was initially developed to follow immune responses over time in clients with mild or moderate COVID. The idea was to record details of a “effective” immune response– one in which clients didnt get too ill, didnt require to be hospitalized, and recovered totally.
However the team quickly understood that even amongst those who didnt get super ill, not everyone recovered. In their preliminary work in 2020 tracing the information of immune responses in 18 COVID clients, the researchers found a handful whose signs continued, early examples of what would eventually be termed long-haul COVID, or simply long COVID.
In those early days of the study, the researchers saw that particular immune responses– particularly swelling– were consistently high in these couple of patients with long COVID. In the patients that got sick and then recovered completely, inflammation levels increased as their bodies battled off the health problem, and after that went back down as they got much better. In those with long COVID, the levels never returned down.
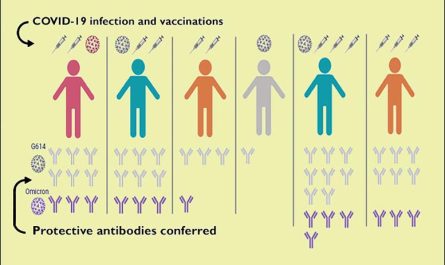
The group decided to broaden their research study to look at more clients with long COVID, focusing on a panel of 1500 proteins flowing in the blood. These assays exposed different molecular “buckets” of long COVID, non-inflammatory and namely inflammatory long COVID. Comprehending the molecular roots of the disease, or subsets of the disease, will help guide clinical trial style and eventually treatment choices, the researchers said.
” The ultimate objective is to deal with patients,” Talla said. “Although we call whatever long COVID, whats come out of this work reveals us that we may not have the ability to provide everybody the exact same type of treatments and we shouldnt put everybody into one group for treatment purposes.”
Those clients with non-inflammatory long COVID may be living with long-term organ or tissue damage from their illness, Torgerson stated. That would require really various treatment from those with high levels of inflammation. The researchers likewise saw that these groups cant be identified based upon symptoms alone. If anti-inflammatory drugs prove efficient in treating inflammatory long COVID, clients would initially need to be screened to identify which type of long COVID they have.
” We hope these findings offer functions of long COVID that might assist prospective future healing techniques,” McElrath said.
Recommendation: “Persistent serum protein signatures specify an inflammatory subcategory of long COVID” by Aarthi Talla, Suhas V. Vasaikar, Gregory Lee Szeto, Maria P. Lemos, Julie L. Czartoski, Hugh MacMillan, Zoe Moodie, Kristen W. Cohen, Lamar B. Fleming, Zachary Thomson, Lauren Okada, Lynne A. Becker, Ernest M. Coffey, Stephen C. De Rosa, Evan W. Newell, Peter J. Skene, Xiaojun Li, Thomas F. Bumol, M. Juliana McElrath and Troy R. Torgerson, 9 June 2023, Nature Communications.DOI: 10.1038/ s41467-023-38682-4.
Out of 55 patients with long COVID, about two-thirds had persistently high levels of certain signals of swelling. The scientists likewise looked at blood samples from 25 people who had COVID however recuperated, and from 25 volunteers who had actually never ever had actually COVID to their knowledge. In those early days of the study, the researchers saw that certain immune actions– particularly inflammation– were regularly high in these couple of clients with long COVID. These assays exposed various molecular “buckets” of long COVID, non-inflammatory and specifically inflammatory long COVID. If anti-inflammatory drugs prove efficient in treating inflammatory long COVID, patients would first need to be screened to identify which kind of long COVID they have.
A research study from the Allen Institute and Fred Hutchinson Cancer Center discovered that an overactive inflammatory response might be a reason for lots of long COVID cases. These findings recommend that certain types of anti-inflammatory drugs could possibly assist reduce symptoms for some clients with long COVID, promoting the idea of precision medication in treating this condition.
The molecular footprint of the chronic condition could provide important insights for assisting clinical trials and treatment techniques.
An increased inflammatory action could be at the root of various cases of long COVID, recommends current research study from the Allen Institute and Fred Hutchinson Cancer.
By analyzing proteins discovered in the blood stream, the researchers recognized a specific group of molecules associated with inflammation. Notably, these particles were exclusively found in a specific group of long COVID patients and were missing in people who had entirely recovered from the infection. The teams findings are detailed in an article recently released in the journal Nature Communications.
Out of 55 clients with long COVID, about two-thirds had persistently high levels of particular signals of swelling. The scientists also took a look at blood samples from 25 individuals who had COVID but recuperated, and from 25 volunteers who had actually never had actually COVID to their knowledge. Those without long COVID did disappoint the same indications of swelling in their blood.