Scattered midline gliomas including DIPG with a mutation called H3K27M are particularly aggressive, with a total survival rate of 11-15 months. These growths are most frequently discovered in kids and young people. The only available treatment is radiation, and even that is challenging as the tumors lie in the middle of brain regions with important functions.
” Its an extremely difficult tumor to treat,” stated senior author Carl Koschmann, M.D., associate professor of pediatric neuro-oncology and medical scientific director of the Chad Carr Pediatric Brain Tumor Center at Michigan Medicine. “Prior to this study, there have been more than 250 scientific trials that have not had the ability to improve results. This is a major fracture in the armor.”
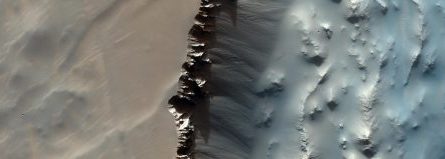
A series of brain scans reveal a growth shrinking in response to ONC201. Credit: Michigan Medicine
In 2 medical trials evaluating ONC201 in a total of 71 clients with H3K27M-mutated scattered midline gliomas, the typical total survival was almost 22 months for tumors that had actually not recurred at the time of enrollment. Almost a 3rd of the clients lived longer than 2 years.
ONC201 took an unusual course to a clinical trial. Initially designed to target dopamine receptors, which are upregulated in lots of different tumors, researchers saw that the drug passes the blood-brain barrier, among the most significant obstacles to developing drugs for brain growths. Initial trials in glioblastoma were not effective, however a little number of patients with DMG that carried the H3K27M mutation had more appealing outcomes. Without understanding why it worked better in these clients, a phase 1 trial was begun in kids and young adults with H3K27M-mutated DMG.
Koschmann and co-author Sriram Venneti, M.D., Ph.D., were trying to figure out what was taking place in these tumor cells.
Through the trial, they collected cerebrospinal fluid from clients. They used this fluid to analyze metabolic modifications and found ONC201 entered the growth cells and impacted mitochondria. Patients who reacted to the drug had a boost in a metabolite called L-2HG produced by growth cells.
Koschmann called the finding “quite unanticipated.” The group discovered that increased L-2HG reversed tumor-defining epigenetic signals triggering growth cells to differentiate more and divide less. The longer patients were on ONC201, the more growths showed these epigenetic reversals.
” This might describe why this patient population was responding so well to the drug since it had this particular epigenetic problem that might be switched off by ONC201. The growths have an epigenetic change triggered by the H3K27M anomaly and ONC201 metabolically reverses that change,” stated Venneti, associate teacher of pathology and pediatrics and clinical research study director of the Chad Carr Pediatric Brain Tumor Center at Michigan Medicine.
Extra scientific trials are currently underway, including screening ONC201 in mix with other treatments. Researchers at U-Ms Chad Carr Pediatric Brain Tumor Center are likewise continuing to look at ways to conquer resistance to ONC201 by utilizing drug mixes.
Koschmann keeps in mind that even a near-doubling of survival is insufficient for households of clients with this medical diagnosis, as the growth remains very deadly. He hopes this very first action will lead to larger leaps in the future.
” For now we have this client population that didnt have a drug before, and now we see much of the growths reacting. We have a platform to develop on and we can likewise describe why its working,” he said.
” We are truly delighted about this study and picture ONC201 becoming the standard of care for these patients in the near future,” Venneti said.
Reference: “Clinical effectiveness of ONC201 in H3K27M-mutant scattered midline gliomas is driven by interruption of incorporated epigenetic and metabolic paths” by Sriram Venneti, Abed Rahman Kawakibi, Sunjong Ji, Sebastian M. Waszak, Stefan R. Sweha, Mateus Mota, Matthew Pun, Akash Deogharkar, Chan Chung, Rohinton S. Tarapore, Samuel Ramage, Andrew Chi, Patrick Y. Wen, Isabel Arrillaga-Romany, Tracy T. Batchelor, Nicholas A. Butowski, Ashley Sumrall, Nicole Shonka, Rebecca A. Harrison, John de Groot, Minesh Mehta, Matthew D. Hall, Doured Daghistani, Timothy F. Cloughesy, Benjamin M. Ellingson, Kevin Beccaria, Pascale Varlet, Michelle M. Kim, Yoshie Umemura, Hugh Garton, Andrea Franson, Jonathan Schwartz, Rajan Jain, Maureen Kachman, Heidi Baum, Charles F. Burant, Sophie L. Mottl, Rodrigo T. Cartaxo, Vishal John, Dana Messinger, Tingting Qin, Erik Peterson, Peter Sajjakulnukit, Karthik Ravi, Alyssa Waugh, Dustin Walling, Yujie Ding, Ziyun Xia, Anna Schwendeman, Debra Hawes, Fusheng Yang, Alexander R. Judkins, Daniel Wahl, Costas A. Lyssiotis, Daniel de la Nava, Marta M. Alonso, Augustine Eze, Jasper Spitzer, Susanne V. Schmidt, Ryan J. Duchatel, Matthew D. Dun, Jason E. Cain, Li Jiang, Sylwia A. Stopka, Gerard Baquer, Michael S. Regan, Mariella G. Filbin, Nathalie Y.R. Agar, Lili Zhao, Chandan Kumar-Sinha, Rajen Mody, Arul Chinnaiyan, Ryo Kurokawa, Drew Pratt, Viveka N. Yadav, Jacques Grill, Cassie Kline, Sabine Mueller, Adam Resnick, Javad Nazarian, Joshua E. Allen, Yazmin Odia, Sharon L. Gardner and Carl Koschmann, 16 August 2023, Cancer Discovery.DOI: 10.1158/ 2159-8290. CD-23-0131.
Financing for this work is from the National Institutes of Health, Department of Defense, University of Michigan Chad Carr Pediatric Brain Tumor Center, The Evans Family, ChadTough Defeat DIPG Foundation, Catching Up with Jack, Pediatric Brain Tumor Foundation, Prayers From Maria Foundation, Michael Miller Memorial Foundation, Morgan Behen Golf Classic, Yuvaan Tiwari Foundation, Sontag Foundation, Alex Lemonade Stand Foundation, Hyundai Hope Foundation, Research Council of Norway, The South-Eastern Norway Regional Health Authority, The University of Oslo, Oncoceutics, Inc., Chimerix, Inc., Making Headway Foundation, Gustave Roussy Foundation Pediatric Campaign, Imagine for Margo Charity, National Research Foundation of Korea, DGIST Start-up Fund, and University of Michigan Taubman Institute.
This work was supported by these Rogel Cancer Center Shared Resources: Experimental Irradiation and Preclinical Molecular Imaging.
” Its an incredibly difficult tumor to deal with,” said senior author Carl Koschmann, M.D., associate professor of pediatric neuro-oncology and medical scientific director of the Chad Carr Pediatric Brain Tumor Center at Michigan Medicine. Developed to target dopamine receptors, which are upregulated in many various growths, researchers saw that the drug passes the blood-brain barrier, one of the most significant difficulties to creating drugs for brain tumors. They used this fluid to analyze metabolic modifications and discovered ONC201 got into the growth cells and impacted mitochondria. Patients who reacted to the drug had an increase in a metabolite called L-2HG produced by growth cells.
The longer clients were on ONC201, the more growths showed these epigenetic turnarounds.
Researchers have found a drug candidate, ONC201, that nearly doubled the survival rate for clients with aggressive childhood brain tumors called scattered midline gliomas (DMG) or diffuse intrinsic pontine glioma (DIPG).
Clinical studies expose extended survival in scattered midline glioma clients receiving ONC201 treatment; research also discusses the underlying system of the drugs success.
For the very first time, a potential drug prospect has been determined by researchers that reveal guarantee in improving outcomes for patients suffering from a specific kind of childhood brain tumor that currently does not have effective treatment options. The compound, called ONC201, was observed to nearly double the survival rates for patients identified with diffuse midline glioma (DMG) or scattered intrinsic pontine glioma (DIPG) when compared to previous patient results.
The findings are reported by a worldwide group of scientists led by the University of Michigan Health Rogel Cancer Center and the Chad Carr Pediatric Brain Tumor.
In addition to reporting on the results of two early-stage medical trials, the paper exposes the hidden mechanisms behind the substances success in these tumors. The paper is released in Cancer Discovery, a journal of the American Association for Cancer Research.