In the 1890s, physician William Coley injected patients who had cancer with bacteria after learning about patients who experienced spontaneous tumor regression following a concurrent bacterial infection.1 He was one of the first scientists to link immune system activation with an antitumor response, which earned him the appellation, “the father of immunotherapy.” Despite some successes in the clinic, safety concerns and the rise of radiotherapy caused these bacterial elixirs, known as Coley’s toxins, to fall by the wayside.
Over the last few decades, advancements across immunology, microbiology, and synthetic biology renewed interest in bioengineering bugs for cancer therapies.2 In a paper published in Science, researchers designed probiotics to colonize tumors and guide engineered T cells to the cancer site.3 Their novel platform not only shows that engineered bacteria can help existing immunotherapies gain access to difficult-to-treat solid tumors, but also highlights the broader potential of living drugs.
Synthetic solutions for solid tumors
The tumor microenvironment is an inhospitable ecosystem. “For bacteria, they kind of don’t care about all of that. They are really, at a very general level, looking for a place where they can survive in the body that’s away from the immune system,” said Tal Danino, a synthetic biologist at Columbia University and author of the study.
The hypoxic, minimally surveilled core of a solid tumor is the perfect bacterial bungalow. However, some bacterial strains can still inhabit healthy organs, so researchers need to explore ways to modify the bacterial genome to reduce virulence and toxicity. Although attenuated bacteria proved safer in both mice and humans, researchers observed poor tumor colonization and no tumor regression.4,5 Now, to improve tumor targeting and specificity, researchers are searching for synthetic biology solutions.
What we’re really excited about is building a platform that other people could use to deliver their payloads or interact with other kinds of cancer modalities that they’re developing.
– Tal Danino, Columbia University
During his graduate studies, Danino built tiny genetic circuits in bacteria that trigger synchronized lysis once the bacteria reach a population density threshold, or quorum, upon which they release genetically-encoded cargo.6 A handful of bacteria fail to burst, seeding the next cycle of growth, quorum, and lysis. “It’s an imperfect system, and that’s kind of the beauty of it,” said Rosa Vincent, a graduate student in Danino’s team and coauthor of the paper. “It’s a cyclical delivery mechanism.”
Danino became interested in using this oscillating gene circuit to tackle biomedical challenges, so he pivoted to bacterial cancer therapies. Bacteria already have a proclivity for the tumor microenvironment, so he focused on engineering the bugs to produce a diagnostic or therapeutic once inside the tumor, akin to a Trojan horse.7,8
“The idea of using the bacteria to tag just a particular location, that’s very promising and overcomes the challenge of antigen heterogeneity,” said Rogelio Hernández-López, a bioengineer at Stanford University who was not involved in the study. One of the reasons solid tumors are difficult to treat using otherwise successful antigen-targeted therapies like chimeric antigen receptor (CAR) T cells is that very few antigens found on the surfaces of tumors are specific to the cancer cells.9 Furthermore, tumor-associated antigens are heterogeneous between patients and cancer cells can mutate to escape targeted therapies, leaving clinicians to hunt down a moving target.
“I started to wonder how we can make a good CAR for a solid tumor if there’s no good target,” said Vincent, who previously worked on logic-gated approaches to target CAR T cells to solid tumors. This curiosity led her to Danino’s work on engineered bacteria for cancer therapy.
See Also “Bacteria as Living Microrobots to Fight Cancer“
For their Trojan horse, the researchers engineered the probiotic strain Escherichia coli Nissle 1917, which was equipped with Danino’s quorum sensing lysis circuit. Once the bacteria reached quorum, they released synthetic antigens that stuck to the tumor. Specifically, the researchers fused a green fluorescent protein (GFP) to the heparin binding domain (HBD) of a placental growth factor protein.10 The sticky HBD anchored to collagens and polysaccharides, ubiquitous components in the tumor environment, thus planting GFP flags on the tumor. Although these molecules are found in healthy tissue, they are highly abundant in the tumor. “We’re entirely relying on the bacteria being specific for these tumors,” Vincent noted.
Most Food and Drug Administration (FDA) approved CAR T cell therapies target the tumor antigen cluster of differentiation 19 (CD19), but Vincent designed her CAR to target their synthetic GFP antigen. “We’re painting the tumors green, and the T cells recognize green,” said Vincent. “The beauty of the CAR is that they’re modular, so you can just swap the antigen binding domain with anything, really,” said Vincent.
When they tested their probiotic CAR system in vitro using different human cancer cell lines, the researchers observed increased specificity and cytotoxicity relative to systems lacking either the GFP tag or receptor. Following the in vitro inspections, their system was ready to leave the garage and hit the road.
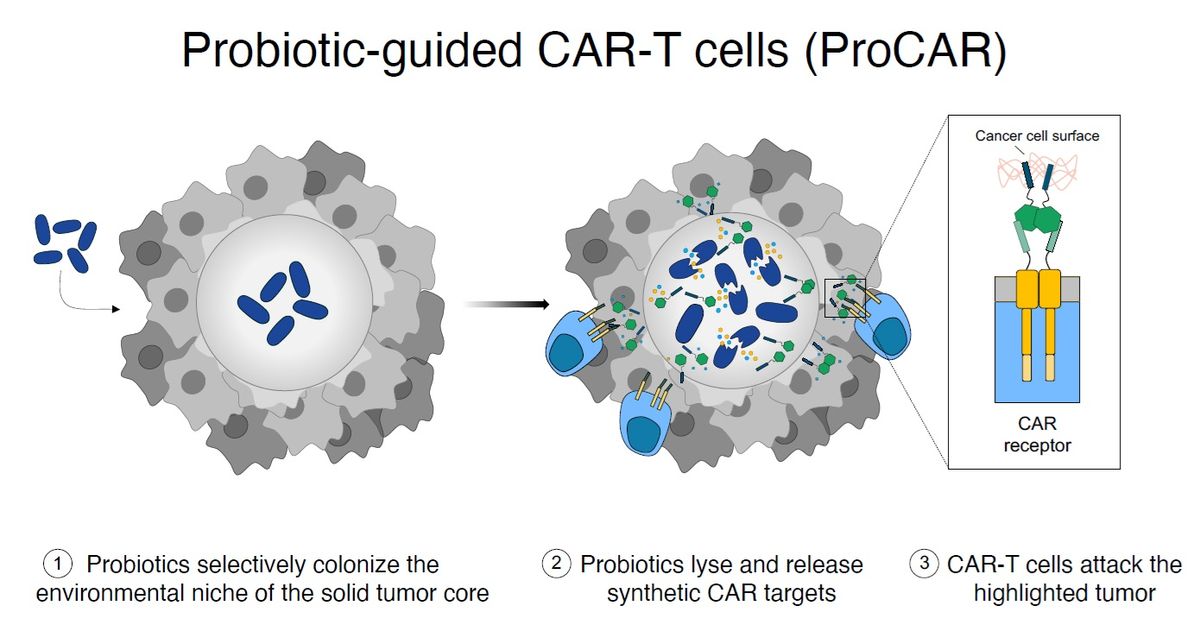
The ProCAR platform combines two engineered systems, probiotics and CAR T cells, to tag solid tumors and guide immune cells to the site.
Rosa Vincent, Columbia Engineering
Taking the probiotic CAR model out for a spin
For the first in vivo test of their probiotic CAR platform, the researchers turned to immunodeficient mice bearing subcutaneous tumors derived from human cancer cells. After injecting the engineered bacteria directly into the tumor, they waited 48 hours to allow for quorum-regulated release of the GFP tags before similarly delivering the engineered CAR.11 The engineered probiotic CAR system inhibited tumor growth, and subsequent flow cytometry analyses of the tumors provided evidence of increased T cell activation.
The researchers also found that a partial system produced a partial response: empty bacteria administered alongside the engineered CAR still triggered some T cell activation at the tumor site. “My favorite part of the system is the fact that the T cells respond really strongly to bacteria,” said Vincent. “[This] puts them as this really desirable partner organism. They can release payloads, yes, but they’re also naturally stimulatory so they’re making a colder tumor hotter.”
To increase CAR T cell proliferation and persistence, patients must first undergo lymphodepletion to kill circulating T cells.12 However, a long-term goal of immunotherapies is to administer the treatment to an intact immune system. “We’re going to need help from the endogenous immune system rather than relying on one antigen to clear the whole tumor,” said Vincent.
To test their system on a functioning immune system, Vincent and her colleagues implanted mouse-derived tumors on both hind flanks of immune-competent mice and then administered the engineered bacteria directly to one of the tumor sites, followed a few days later by two rounds of CAR T treatment. (They introduced an extra dose of CAR T cells to combat T cell exhaustion.) The researchers hoped that their system could generate enough inflammation to stimulate the host immune system to recognize the additional tumor, so they were excited to find a reduction in tumor growth in not only the treated tumor but also the untreated site.
See Also “Helping Engineered T Cells Find Their Way to Tumors“
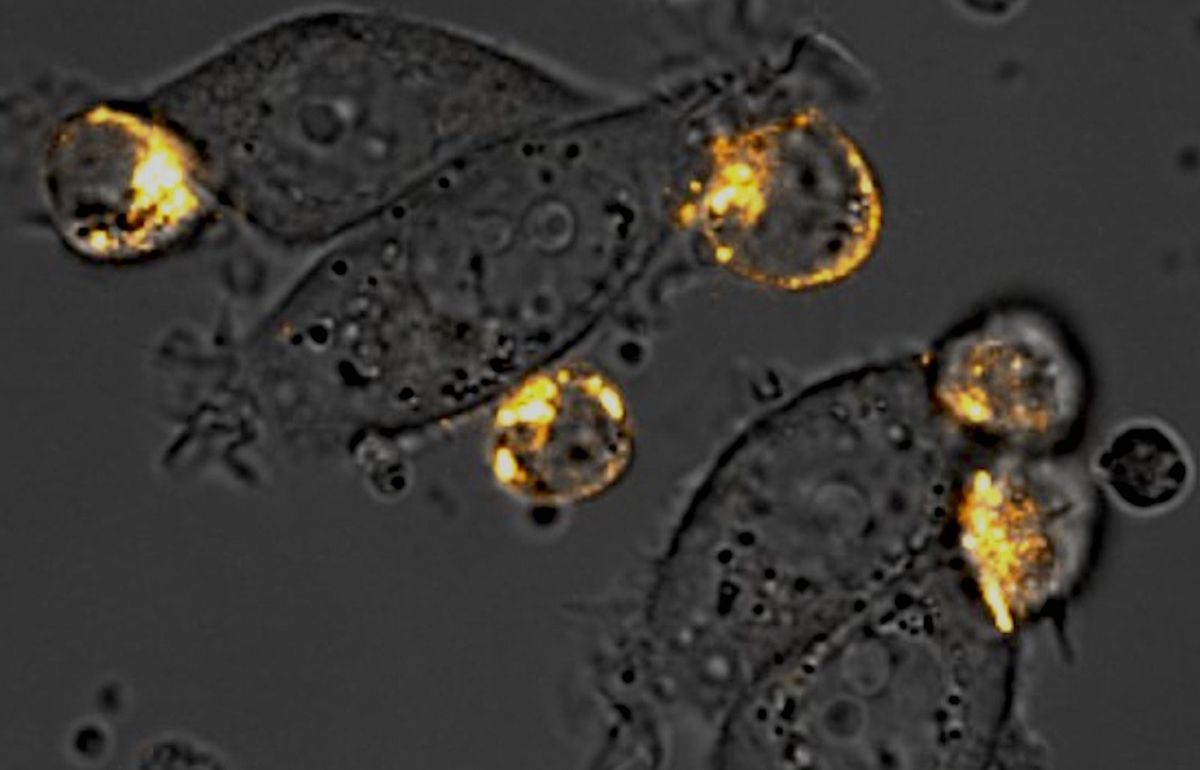
Researchers engineered their CAR (in orange) to express a receptor for the synthetic GFP antigen released by bacteria after colonizing the solid tumor.
Rosa Vincent and Thomas Savage, Columbia Engineering
The subcutaneous experiments prepared for the big experiment: intravenous administration of the probiotic CAR system. For this, they implanted human cancer cells into the mammary fat pads of mice with weakened immune systems and then administered the probiotic CAR regimen with one small tweak to the system. In order to further coax the CAR T cells to the tumor site, the researchers engineered the bacteria to corelease the immune cell attractant human chemokine ligand 16 (CXCL16).13 This paved a concentration gradient for the CAR T cells to drive along towards the tumor. The added chemokine cargo added a boost to the system, outperforming the standard probiotic CAR regimen with respect to tumor growth inhibition. Additionally, analyses of other organs showed that bacteria and GFP expression was restricted to the tumor site.
Before transitioning these experiments to humans, the researchers will first need to genetically attenuate their engineered bacteria. In this study, they used a wild type strain of E coli, but mice are less sensitive than humans to Gram-negative bacteria toxicity.14 “The major focus of the lab now is trying to make a translational strain of bacteria,” said Vincent.
A synthetic space for the growth of bacterial therapies
“This is an example of how two different engineered systems can be complementary and synergize their function,” said Hernández-López. “[Danino] has been developing the circuit to lyse bacteria for many years and it’s great to see it now in combination with other approaches.”
When Danino sees bacteria, he sees a versatile platform that can deliver therapeutics to tumors but also interact with other modalities. Beyond remodeling the tumor environment to boost CAR T efficacy, researchers are exploring how engineered bacteria can enhance positron emission tomography (PET)/magnetic resonance imaging (MRI), focus ultrasounds, and even deliver drug-loaded nanoparticles.15 “What we’re really excited about is building a platform that other people could use to deliver their payloads or interact with other kinds of cancer modalities that they’re developing,” said Danino.
“The microbiome engineering field is slowly converging towards meeting the engineered T cell field, and it’s going to be exciting to see what comes next,” said Hernández-López.
References
- Hoption Cann SA, et al. Dr William Coley and tumour regression: A place in history or in the future. Postgrad Med J. 2003;79(938):672-680.
- Duong MTQ, et al. Bacteria-cancer interactions: Bacteria-based cancer therapy. Exp Mol Med. 2019;51:1-15.
- Vincent RL, et al. Probiotic-guided CAR-T cells for solid tumor targeting. Science. 2023;382(6667):211-218.
- Low KB, et al. Lipid A mutant Salmonella with suppressed virulence and TNFα induction retain tumor-targeting in vivo. Nat Biotechnol. 1999;17:37-41.
- Toso JF, et al. Phase I study of the intravenous administration of attenuated Salmonella typhimurium to patients with metastatic melanoma. J Clin Oncol. 2002;20(1):142-152.
- Din MO, et al. Synchronized cycles of bacterial lysis for in vivo delivery. Nature. 2016;536:81-85.
- Danino T, et al. Programmable probiotics for detection of cancer in urine. Sci Transl Med. 2015;7(289):289ra84.
- Chowdhury S, et al. Programmable bacteria induce durable tumor regression and systemic antitumor immunity. Nat Med. 2019;25:1057-1063.
- Albelda SM. CAR T cell therapy for patients with solid tumors: Key lessons to learn and unlearn. Nat Rev Clin Oncol. 2023;21(1):47-66.
- Martino MM, et al. Growth factors engineered for super-affinity to the extracellular matrix enhance tissue healing. Science. 2014;343(6173):885-888.
- Gurbatri CR, et al. Engineered probiotics for local tumor delivery of checkpoint-blockade nanobodies. Sci Transl Med. 2020;12(530):eaax0876.
- Amini L, et al. Preparing for CAR T cell therapy: Patient selection, bridging therapies and lymphodepletion. Nat Rev Clin Oncol. 2022;19:342-355.
- Savage TM, et al. Chemokines expressed by engineered bacteria recruit and orchestrate antitumor immunity. Sci Adv. 2023;9(10):eadc9436.
- Copeland S, et al. Acute inflammatory response to endotoxin in mice and humans. Clin Diagn Lab Immunol. 2005;12(1):60-67.
- Gurbatri CR, et al. Engineering bacteria as interactive cancer therapies. Science. 2022;378(6622):858-864.

