Breast cancer is a condition where breast cells multiply uncontrollably.
Together, diabetes and breast cancer can posture a serious danger
Type 2 diabetes and breast cancer would appear to be extremely various conditions, sharing nothing but their commonness. In the United States, 1 in 8 women will develop intrusive breast cancer throughout their lifetime, making it the second usually identified malignancy after numerous kinds of skin cancer. More than 10% of Americans have diabetes, and 2 in 5 are anticipated to get the persistent illness at some point in their lives.
Previous research studies have shown connections in between the two conditions. For circumstances, the danger of breast cancer in ladies with diabetes is increased by 20– 27%. Insulin resistance, a major attribute of diabetes, has been connected to an increased occurrence of breast cancer and a worse opportunity of survival. According to population research studies, diabetes danger increases 2 years after a breast cancer medical diagnosis and is 20% higher in breast cancer survivors than in age-matched ladies without the disease by the end of the first years after the diagnosis.
These epidemiological connections, however, are unclear or definitive, and other investigations have actually revealed no relationships at all. Scientists from the University of California San Diego School of Medicine explain a potential biological system linking the 2 diseases, in which breast cancer suppresses the production of insulin, triggering diabetes and the degeneration of blood sugar control which encourages tumor growth. The research study was just recently released in Nature Cell Biology.
In the United States, 1 in 8 females will establish intrusive breast cancer throughout their life time, making it the second most frequently diagnosed malignancy after different kinds of skin cancer. Insulin resistance, a significant attribute of diabetes, has actually been connected to an increased incidence of breast cancer and a worse possibility of survival. According to population studies, diabetes danger increases 2 years after a breast cancer medical diagnosis and is 20% greater in breast cancer survivors than in age-matched ladies without the illness by the end of the first years after the diagnosis.
Scientists from the University of California San Diego School of Medicine describe a possible biological system connecting the 2 illness, in which breast cancer reduces the production of insulin, causing diabetes and the deterioration of blood sugar control which motivates tumor development. By increasing blood glucose that can be easily utilized by cancer cells, breast tumors make their own favorite food and, meanwhile, deny this vital nutrient from typical cells.”
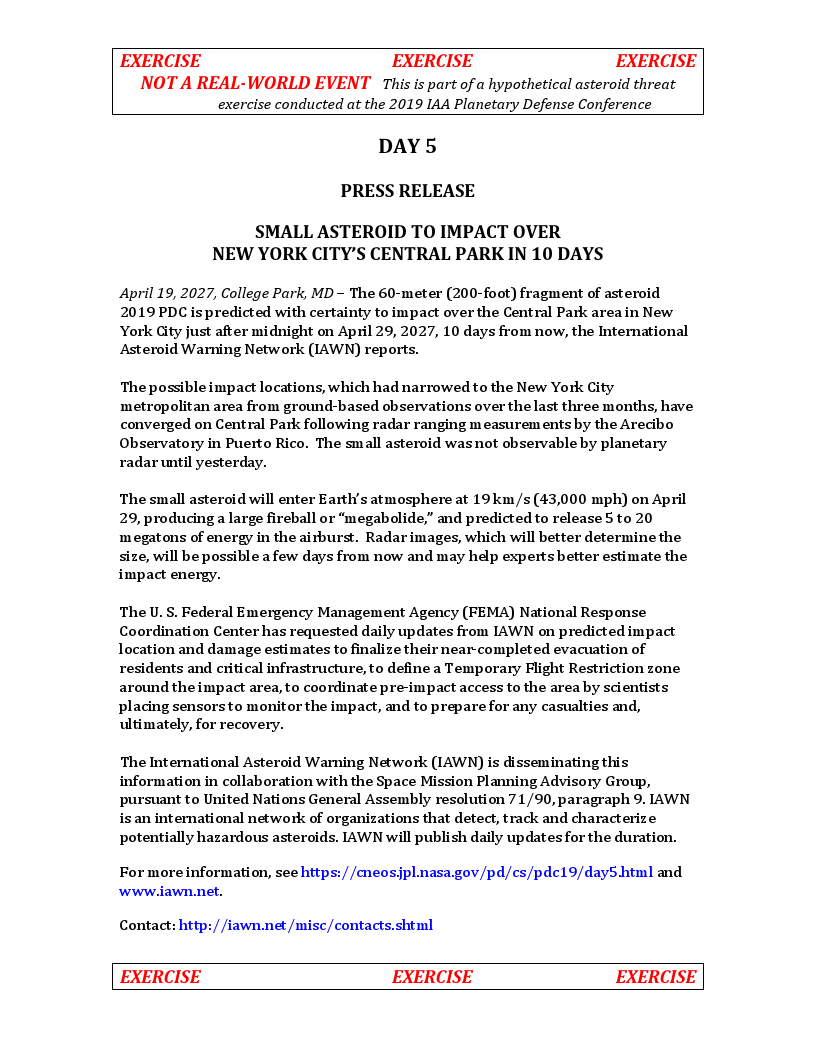
A breast cancer cell recorded in the process of division, with tubulin (a structural protein) in red; mitochondria in green; and chromosomes in blue. Credit: Wei QianNational Cancer Institute
” No illness is an island because no cell lives alone,” said corresponding research study author Shizhen Emily Wang, Ph.D., professor of pathology at UC San Diego School of Medicine. “In this research study, we describe how breast cancer cells hinder the function of pancreatic islets to make them produce less insulin than needed, resulting in greater blood glucose levels in breast cancer clients compared to women without cancer.”
Wang said the research study was inspired by early work and assistance from Jerrold Olefsky, MD, professor of medication and associate dean for scientific affairs in the Division of Endocrinology and Metabolism at UC San Diego School of Medicine. Olefsky is the co-senior author of the research study with Wang.
The culprit, according to Wang and Olefsky, are extracellular vesicles (EV)– hollow spheres secreted or shed by cells that transfer DNA, RNA, proteins, fats, and other products between cells, a sort of cargo interaction system.
In this case, the cancer cells were found to be secreting microRNA-122 into the vesicles. Wang said when blisters reach the pancreas, they can go into the islet cells accountable for insulin production, dispense their miR-122 cargo and damage the islets critical function in maintaining a regular blood glucose level.
” Cancer cells have a sweet tooth,” Wang said. “They utilize more glucose than healthy cells in order to fuel tumor development, and this has actually been the basis for PET scans in cancer detection. By increasing blood sugar that can be easily utilized by cancer cells, breast tumors make their own favorite food and, meanwhile, deprive this necessary nutrient from normal cells.”
The research study was conducted utilizing mouse models, which found that slow-releasing insulin pellets or a glucose-lowering drug referred to as an SGLT2 inhibitor brought back normal control of glucose in the presence of a breast tumor, which in turn suppressed the tumors development.
” These miR-122 inhibitors, which happen to be the very first miRNA-based drugs to get in scientific trials, may have a new use in breast cancer treatment,” Wang stated.
The research study was moneyed by the NIH/National Institutes of Health and the Hartwell Foundation..
Recommendation: “Cancer-cell-secreted extracellular blisters suppress insulin secretion through miR-122 to impair systemic glucose homeostasis and contribute to tumour development” by Minghui Cao, Roi Isaac, Wei Yan, Xianhui Ruan, Li Jiang, Yuhao Wan, Jessica Wang, Emily Wang, Christine Caron, Steven Neben, Denis Drygin, Donald P. Pizzo, Xiwei Wu, Xuxiang Liu, Andrew R. Chin, Miranda Y. Fong, Ziting Gao, Kaizhu Guo, Oluwole Fadare, Richard B. Schwab, Yuan Yuan, Susan E. Yost, Joanne Mortimer, Wenwan Zhong, Wei Ying, Jack D. Bui, Dorothy D. Sears, Jerrold M. Olefsky, and Shizhen Emily Wang, 30 May 2022, Nature Cell Biology.DOI: 10.1038/ s41556-022-00919-7.