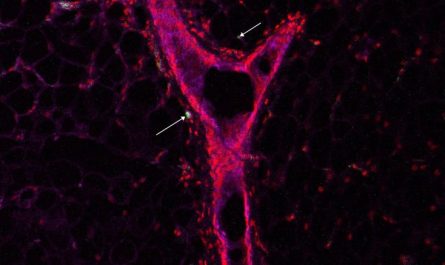
A brand-new study published in Neurology has actually discovered a correlation between extreme sleep apnea and lower brain volumes in the median temporal lobe location, including the hippocampus, in individuals with amyloid plaques, an early sign of Alzheimers disease. This correlation, which might suggest brain cell loss, was not seen in those without plaques. The study, nevertheless, does not establish causality between sleep apnea and lower brain volume.
A current research study has discovered an association in between serious sleep apnea and decreased brain volume in regions important to memory in individuals with early signs of Alzheimers disease. The study stresses the need for further research into sleep-disordered breathing treatments to potentially enhance cognition and hold-up neurodegeneration.
Studies have actually shown that sleep apnea is related to an increased threat of dementia. A new research study takes a look at the relationship between sleep apnea and brain volume. The research study is published in the May 31, 2023, online problem of Neurology, the medical journal of the American Academy of Neurology.
The research study compared people who have amyloid plaques in the brain that are an early sign of Alzheimers illness however do not have any memory problems to people with no amyloid plaques.
A brand-new research study published in Neurology has actually discovered a connection between serious sleep apnea and lower brain volumes in the medial temporal lobe location, including the hippocampus, in individuals with amyloid plaques, an early sign of Alzheimers illness. The study, however, does not establish causality in between sleep apnea and lower brain volume.
A brand-new research study looks at the relationship between sleep apnea and brain volume. Participants had brain scans, took tests of their memory and had an over night sleep study done in their homes.
” We discovered that people with amyloid plaques who had more severe sleep apneas likewise were more most likely to have lower volumes in the median temporal lobe area of the brain, including the hippocampus, which contributes in memory and Alzheimers illness,” said research study author Geraldine Rauchs, PhD, of Inserm in Caen, France. “The people who did not have amyloid plaques did not have this lower brain volume, even if they had serious sleep apneas.”
The study does not prove that sleep apnea triggers lower brain volume; it only shows an association.
The study included 122 people with an average age of 69 who did not have memory issues. Individuals had brain scans, took tests of their memory and had an overnight sleep study done in their homes.
In people with amyloid plaques, having more extreme sleep apneas was connected with having lower brain volume in the medial temporal lobe area of the brain which may recommend loss of brain cells. This connection was not discovered in people who did not have amyloid plaques.
” Our results recommend that some individuals might be more susceptible to the adverse effects of sleep apnea,” Rauchs said. “People who are in the extremely early stages of the Alzheimers continuum showed a specific vulnerability to sleep apneas. Additional research studies need to look at whether treating sleep-disordered breathing could potentially enhance cognition and postpone or prevent neurodegeneration.”.
In the whole group, lower volumes in the hippocampus at the beginning of the study were associated with lower ratings on a test of episodic memory at the end of the research study.
There were no associations between sleep apneas at the start of the study and memory scores at the end of the study.
A constraint of the research study was that the very same version of the verbal knowing test was provided at the start and end of the study, so its possible that some memory decrease may have been lessened due to familiarity with the test.
Recommendation: “Association of Sleep-Disordered Breathing and Medial Temporal Lobe Atrophy in Cognitively Unimpaired Amyloid-Positive Older Adults” by Claire André, Elizabeth Kuhn, Stéphane Rehel, Valentin Ourry, Solène Demeilliez-Servouin, Cassandre Palix, Francesca Felisatti, Pierre Champetier, Sophie Dautricourt, Paul Yushkevich, Denis Vivien, Vincent de La Sayette, Gaël Chételat, Robin de Flores and Géraldine RAUCHS, for the Medit-Ageing Research Group, 31 May 2023, Neurology.DOI: 10.1212/ WNL.0000000000207421.
The research study was supported by the European Unions Horizon 2020 Research and Innovation Program, Inserm, Region Normandy, and the MMA Corporate Foundation of Entrepreneurs of the Future (Fondation dEntreprise MMA des Entrepreneurs du Futur).